Return-to-Play: The importance of pre-season concussion baseline testing for high-risk contact athletes.
It might be early (or late) to be thinking about this, depending on when you’re reading this. But, this is an important discussion, especially with rising awareness around concussion. As a concussion specialist, much of this awareness is a mixed bag of, “I’m so glad people are talking about this!” and, “Woah, woah, woah! They’ve got that way wrong.”
For example, I’m happy we’re talking about concussion risks, but we flat out do not know as much about CTE as various documentaries and The New York Times would want you to believe. Preemptively removing children from/* canceling sports would likely cause more harm than good in the long game of social and physical development of these athletes. There are actually societal benefits achieved from youth sports.
*Wouldn’t we also have to find a way to cancel falls, car accidents, blast injuries and all other forms of concussion?
Rather than removing sports, why don’t we...?
Educate parents, coaches, and athletes about signs/symptoms of concussion.
Educate parents, coaches, and athletes about concussion metabolism and recovery.
De-stigmatized (and de-penalize) concussion reporting among athletes.
Follow recommended, evidence-based treatment guidelines.
Use objective, multimodal testing to ensure an appropriate and safe return to sport after a concussion.
Here’s what we’ll likely see with those measures:
There will be no such thing as a 7-day return-to-play.
Athletes will be more quickly evaluated, diagnosed, and routed to active rehabilitation.
Most athletes will safely return-to-play within 4-8 weeks based upon objective testing.
Is that great for professional sports, fantasy teams, or playoffs? No. But it should still be the gold-standard.
Does it provide a far safer, more evidence-based, and less radical means of addressing youth sport-related concussion? Absolutely. That’s why it should be the gold-standard across all age groups and tiers.
This all starts with a pre-season baseline test.
If society, at large, wants to minimize the long-term risk and damage from concussion, then the return-to-play decisions need to be made more stringently. And that’s going to happen with better, more comprehensive baseline testing.
Baseline testing is not for concussion diagnosis. Most of the time concussion diagnosis is relatively easy in sport. Baseline testing is what will allow parents, coaches, and athletes to feel confident and safe in their decision to return to sport because now we have metrics (i.e., baseline tests) for how the concussion affected the athlete and where they need to be to return to pre-concussion symptoms and performance.
One reason it’s important to have this “you vs. you” testing in sport is that normative values for baseline tests are often as good as flipping coins. So, when we’re evaluating an athlete for a mid-season concussion without baseline metrics - we might as well flip a coin to decide if their balance, executive function, reaction time, etc… have improved or not.
Think about it this way. Balance is often affected in concussion, and is also needed for performance in most high-risk contact sports.
Let’s look at a scenario where neither athlete A or B have baseline tests:
Athlete A has phenomenal (99th percentile) balance at baseline.
Athlete B has poor (5th percentile) balance at baseline.
With no baseline test, using normative values:
We deem athlete A fit for return because their balance reached the 75th percentile based on normative values.
We deem athlete B unfit for return because their balance is stuck at the 5th percentile based on normative values.
We allowed athlete A to return to sport before they were fully recovered, and we held back athlete B from sport because we didn’t know that was their normal.
Baseline testing allows us to take the guesswork out of return-to-play decisions. We know what they look like healthy, we can track what was impacted when concussed, and we can monitor recovery back to (or better than) baseline during rehab.
Problems with individual baseline tests.
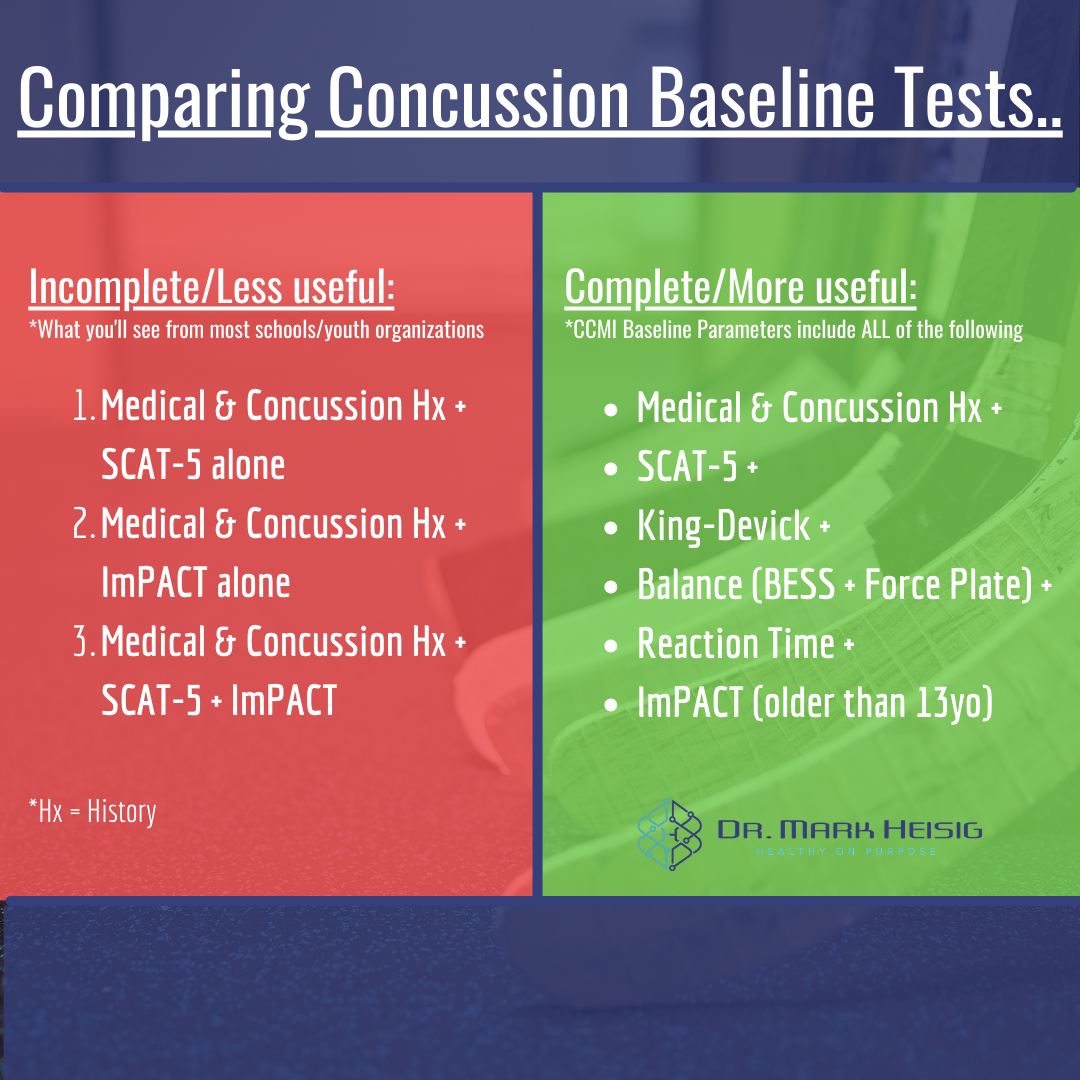
Most youth and high school organizations will talk about their concussion program or partnerships, and athletes will have to undergo “baseline testing” as a part of those programs. The problem is that a vast majority of these organizations will use a single test, most commonly the SCAT-5 or ImPACT, as their baseline protocol - which is advised against in the research. Despite this, roughly 70% of U.S. high schools use an ImPACT only.
Why is it advised against using single tests? Because single tests have poorer test/retest reliability and have different normalization rates.
What does that mean in plain English?
Test/Retest reliability means that when we test someone pre-season, we need that test to be accurate and reliable when the injury happens mid-to-late season. And we need to be able to use that test to make a decision after recovery and rehab have taken place.
Normalization rate refers to how fast any given baseline test will normalize after a concussion - even without symptom resolution or treatment. We need tests that can be used for the duration of concussion recovery.
As an example, the SCAT-5 normalizes within 3 days after a concussion. To put perspective on that, symptoms usually don’t go away for 7-10 days and brain metabolism isn’t normalized for approximately 30 days. Further, we can objectively track and quantify neurocognitive and vestibulo-ocular deficits for 3-4 weeks after a concussion. Regarding the ImPACT testing, we see normative values are as good as flipping coins, and the ImPACT test is not validated for children under 13 years old.
So, when an organization is using, singly, a SCAT-5 or ImPACT for return-to-play decisions, they’re actually making a dangerous guess as to whether the athlete is ready to play or not. (So, is it the sport that should be canceled or the incomplete medical management?)
Quality baseline testing battery.
We know that single tests are advised against in the research for use as sole baseline tests or return-to-play markers. Given that, what are the markers that should be included in a comprehensive baseline test?
This protocol comes from Complete Concussion Management and is arguably the best baseline battery recommended to date. The recommended baseline includes all of the following and takes ~30min to administer:
Medical & Concussion History
SCAT-5
PCSS (Symptom Score)
Orientation
Immediate & Delayed Memory
BESS (Balance)
King-Devick
Force Plate Postural Sway (Balance)
Reaction Time
ImPACT (for folks 13yo and older) - Performed by the athlete on their own time at a computer.
Below are details of this protocol.
The SCAT-5 includes the PCSS and the SAC (Standard Assessment of Concussion). These evaluations are great for sideline diagnosis of concussion, but as mentioned earlier, normalize within the first few days after injury. The utility in these tests, however, is that any drop (even 1pt) from baseline is considered significant. When paired with balance and King-Devick tests, diagnostic accuracy goes way up. Hence, the need for multimodal assessment.
The King-Devick (KD) is the only test in this protocol that assesses oculomotor function by assessing the speed someone can read through scattered numbers left-to-right, top-to-bottom. A drop of 5sec from baseline is significant for concussion, and the validity of the KD test lasts long enough to be useful in return-to-play decisions.
Balance is assessed through two different means, the BESS and a force plate measuring postural sway. The BESS pairs well with the SCAT-5 and KD tests, but normalizes within the week from injury. Thus, it’s also recommended that postural sway be added as a more objective marker, and one that is reliable well into the recovery and return-to-play timeline.
Reaction time is a simple, very relevant neurocognitive marker of athletic performance. Data shows that reaction time can be delayed for 21-59 days after injury, thus making it a durable enough marker to last through the recovery and return-to-play timeline (e.g., if reaction time improves to baseline in 33 days, then it likely HAS recovered and this is a positive mark towards returning to play).
The ImPACT test is an objective, standardized and computerized neurocognitive test useful for folks older than 13 years old. Even asymptomatic concussion patients can still show at least 1 neurocognitive impairment, and as said earlier, we can detect impairments for up to 4 weeks after a concussion. ImPACT was able to detect deficits in 1 of 4 athletes who had been returned-to-play by physicians using the SCAT, thus proving useful in making decisions. However, used alone, the ImPACT is not enough to make a return-to-play decision, but in conjunction with the rest of this protocol it complements the whole nicely.
Making the return-to-play decision.
Keeping in mind our initial goals of minimizing long-term concussion risk in athletes, the decision to return to play should be stringent. We don’t want athletes returning at high risks of repeat concussion or other orthopedic injuries. We want them fresh, performing like themselves (or better), and safely ready to return. Thus, the athlete should be able to meet or exceed their baseline test results before being allowed to return to play, and the baseline needs to be comprehensive enough to capture long-lasting parameters of performance.
One of the ways that we make this sport-specific and truly thorough is by placing aerobic and highly-conditioned athletes (e.g., ice hockey, soccer, lacrosse, MMA, certain positions in football, etc..) through an exertion protocol in the minutes prior to baseline re-testing. This has been able to show 28% more neurocognitive deficits than testing at rest. This sort of testing protocol should make sense to you as the reader; we want to know that our athletes are capable of performing under sport conditions, safely in an office/gym, before we return them to sport where they risk re-injury.
This sort of testing is less relevant in someone like a baseball player or downhill skier. While conditioned and strong, undoubtedly, the cardioautonomic demands are just not the same for a baseball player as they are for an ice hockey player.
That’s me (#17), circa 2012, playing for the NAU Ice Jacks in the ACHA. I sustained 2 unmanaged concussions that season.
Closing the case for comprehensive baseline testing.
Let’s bring it back to the top. We want our athletes safe and performing at their best. The potential concerns around long-term, repeated concussions are (at this time) not concretely known - but still not desired.
What’s the best way to minimize these long-term concussion risks?
Educate parents, coaches, and athletes about signs/symptoms of concussion.
Educate parents, coaches, and athletes about concussion metabolism and recovery.
De-stigmatized (and de-penalize) concussion reporting among athletes.
Follow recommended, evidence-based treatment guidelines.
Use objective, multimodal testing to ensure an appropriate and safe return to sport after a concussion.
Ideally, in the appropriate athletes, these return-to-play baseline tests are performed following an exertion protocol that mimics game conditions.
The athlete who can meet, or exceed, their own baseline markers following an exertion protocol after concussion rehab is the athlete that we can all safely assume is truly recovered and ready to play. We’ve thrown everything in the book at them, plus an anaerobic exertion protocol, and they still showed up and performed as well as their healthy pre-season selves.
That’s an athlete that took 4-8 weeks away from gameplay, participated in rehab/workouts and non-contact practice, and returned when it was proven safe for them to do so. As a provider, I couldn't ask for anything more.
Dr. Mark Heisig is a licensed naturopathic doctor with continuing mTBI education from The American Academy of Neurology (AAN), Complete Concussion. Management (CCMI) and The Carrick Institute. His office is located in Scottsdale, AZ.
References (provided by CCMI Baseline Evidence Sheet):
Giza CC, Hovda DA. The New Neurometabolic Cascade of Concussion. Neurosurgery. 2014;75:S24–S33.
Signoretti S, Lazzarino G, Tavazzi B, Vagnozzi R. The Pathophysiology of Concussion. PM&R. 2011;3(10):S359–68.
Vagnozzi R, Tavazzi B, Signoretti S, Amorini AM, Belli A, Cimatti M, et al. Temporal window of metabolic brain vulnerability to concussions. Neurosurgery. 2007;61(2):379–89.
Vagnozzi R, Signoretti S, Tavazzi B, Cimatti M, Amorini AM, Donzelli S, et al. Hypothesis of the Postconcussive Vulnerable Brain: Experimental Evidence of Its Metabolic Occurrence. Neurosurgery. 2005;57(1):164–71.
Vagnozzi R, Signoretti S, Cristofori L, Alessandrini F, Floris R, Isgro E, et al. Assessment of metabolic brain damage and recovery following mild traumatic brain injury: a multicentre, proton magnetic resonance spectroscopic study in concussed patients. Brain. 2010;133(11):3232–42.
Vagnozzi RR, Signoretti SS, Tavazzi BB, Floris RR, Ludovici AA, Marziali SS, et al. Temporal window of metabolic brain vulnerability to concussion: a pilot 1Hmagnetic resonance spectroscopic study in concussed athletes--part III. Neurosurgery 2008;62(6):1286–6.
Signoretti S, Vagnozzi R, Tavazzi B, Lazzarino G. Biochemical and neurochemical sequelae following mild traumatic brain injury- summary of experimental data and clinical implications. Neurosurg Focus. 2010;29(5):1–12.
Baker JG, Freitas MS, Leddy JJ, Kozlowski KF, Willer BS. Return to Full Functioning after Graded Exercise Assessment and Progressive Exercise Treatment of Postconcussion Syndrome. Rehabilitation Research and Practice. 2012;2012:1–7.
Leddy JJ, Baker JG, Kozlowski K, Bisson L, Willer B. Reliability of a graded exercise test for assessing recovery from concussion. Clin J Sport Med. 2011;21(2):89–94.
Len TK, Neary JP. Cerebrovascular pathophysiology following mild traumatic brain injury. Clinical Physiology and Functional Imaging 2011;31:85-93.
Whyte EF, Gibbons N, Kerr G, Moran KA. The Effect of a High Intensity, Intermittent Exercise Protocol on Neurocognitive Function in Healthy Adults:Implications for Return to Play Management Following Sport Related Concussion. J Sport Rehabil. 2014 (Epub ahead of print).
McGrath N, Dinn WM, Collins MW, Lovell MR, Elbin RJ, Kontos AP. Post-exertion neurocognitive test failure among student-athletes following concussion. Brain Inj. 2013;27(1):103–13.
Vartiainen MV, Holm A, Lukander J, Lukander K, Koskinen S, Bornstein R, et al. A novel approach to sports concussion assessment: Computerized multilimb reaction times and balance control testing. J Clin ExpNeuropsychol. 2015;1–15.
McCrory P, Meeuwisse WH, Aubry M, Cantu B, Dvorak J, Echemendia RJ, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2013;47(5):250–8.
McCrea M, Barr WB, Guskiewicz K, Randolph C, Marshall SW, Cantu R, et al. Standard regression-based methods for measuring recovery after sport-related concussion.J of Int Neuropsychol Soc 2005;11:58–69.
Naunheim RS, Matero D, Fucetola R. Assessment of patients with mild concussion in the emergency department. Journal of Head Trauma Rehabilitation. 2008;23(2):116–22.
McCrea M, Guskiewicz KM, Marshall SW, Barr W, Randolph C, Cantu RC, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003 Nov 19;290(19):2556–63.
McCrea M. Standardized mental status testing on the sideline after sport-related concussion. J Athl Train. 2001.
Baird JT. An effective tool in establishing the diagnosis of sport-related concussion. Journal of the American Academy of Physician …. 2011.
Barr WB, McCrea M. Sensitivity and specificity of standardized neurocognitive testing immediately following sports concussion. J Int Neuropsychol Soc. 2001 Sep 1;7(6):693–702.
Marinides Z, Galetta KM, Andrews CN, Wilson JA, Herman DC, Robinson CD, et al. Vision testing is additive to the sideline assessment of sports-related concussion. Neurology: Clinical Practice. 2015 Feb 16;5(1):25–34.
Dhawan P, Starling A, Tapsell L, Adler J, Galetta S. King-Devick Test Identifies Symptomatic Concussion in Real-time and Asymptomatic Concussion Over Time.(S11. 003). Neurology. 2014.
Leong DF, Balcer LJ, Galetta SL, Evans G, Gimre M, Watt D. Journal of Optometry. 2015 (Epub ahead of print)
Galetta KM, Morganroth J, Moehringer N, Mueller B, Hasanaj L, Webb N, et al. Adding Vision to Concussion Testing. Journal of Neuro-Ophthalmology. 2015 (Epub ahead of print).
Galetta KM, Brandes LE, Maki K, Dziemianowicz MS, Laudano E, Allen M, et al. The King–Devick test and sports-related concussion: Study of a rapid visual screening tool in a collegiate cohort. Journal of the Neurological Sciences. 2011 Oct;309(1-2):34–9.
Riemann BL, Guskiewicz KM, Shields EW. Relationship Between Clinical and Forceplate Measures of Postural Stability. J Sport Rehabil 1999;8:71-82.
Riemann BL, Guskiewicz KM. Effects of mild head injury on postural stability as measured through clinical balance testing. J Athl Train. 2000 Jan 1;35(1):19–25.
Snyder AR, Bauer RM, Health IMPACTS for Florida Network. A Normative Study of the Sport Concussion Assessment Tool (SCAT2) in Children and Adolescents. The Clinical Neuropsychologist. 2014 (Epub ahead of print).
Jinguji TM, Bompadre V, Harmon KG, Satchell EK, Gilbert K, Wild J, et al. Sport Concussion Assessment Tool - 2: Baseline Values for High School Athletes. British Journal of Sports Medicine. 2012 Mar 22;46(5):365–70.
Murray N, Salvatore A, Powell D, Reed-Jones R. Reliability and Validity Evidence of Multiple Balance Assessments in Athletes With a Concussion. J Athl Train. 2014;49(3):540-9.
Buckley T, Evans K, Munkasy B. Lingering Impairments in Postural Control Despite Clinical Concussion Recovery (S27. 001). Neurology. 2015.
Slobounov S, Slobounov E, Sebastianelli W, Cao C, Newell K. Differential rate of recovery in athletes after first and second concussion episodes. Neurosurgery. 2007;61(2):338–44.
Eckner JT, Kutcher JS, Broglio SP, Richardson JK. Effect of sport-related concussion on clinically measured simple reaction time. Br J Sports Med. 2014; 48(2):112-8.
Eckner JT, Kutcher JS, Richardson JK. Effect of Concussion on Clinically Measured Reaction Time in 9 NCAA Division I Collegiate Athletes: A Preliminary Study. PM&R. 2011;3(3):212–8.
Eckner JT, Kutcher JS, Richardson JK. Pilot evaluation of a novel clinical test of reaction time in National Collegiate Athletic Association Division I football players. J Athl Train. National Athletic Trainers Association; 2010;45(4):327.
Eckner JT, Lipps DB, Richardson JK, Ashton-Miller JA. Can a Clinical Test of Reaction Time Predict Functional Head-Protective Response? Medicine & Science in Sports & Exercise. 2011;43(3):382–7.
Eckner JT, Kutcher JS, Richardson JK. Between-Seasons Test-Retest Reliability of Clinically Measured Reaction Time in National Collegiate Athletic Association Division I Athletes. J Athl Train. National Athletic Trainers' Association; 2011;46(4):409–14.
Schatz P, Robertshaw S. Comparing Post-Concussive Neurocognitive Test Data to Normative Data Presents Risks for Under-Classifying “Above Average” Athletes. Archives of Clinical Neuropsychology. 2014 Oct 15;29(7):625–32.
Broglio SP, Ferrara MS, Macciocchi SN, Baumgartner TA, Elliott R. Test-retest reliability of computerized concussion assessment programs. J Athl Train. 2007 Oct;42(4):509–14.
Resch J, Driscoll A, McCaffrey N, Brown C, Ferrara MS, Macciocchi S, et al. ImPact Test-Retest Reliability: Reliably Unreliable? J Athl Train. 2013 Jul;48(4):506–11.
Kontos AP, Braithwaite R, Dakan S, Elbin RJ. Computerized Neurocognitive Testing within 1 Week of Sport-Related Concussion: Meta-analytic Review and Analysis of Moderating Factors. J Int Neuropsychol Soc. 2014 Feb 13;20(03):324–32.
Harmon KG, Drezner JA, Gammons M, Guskiewicz KM, Halstead M, Herring SA, et al. American Medical Society for Sports Medicine position statement: concussion in sport. British Journal of Sports Medicine. 2012 Dec 13;47(1):15–26.
Mayers LB, Redick TS. Clinical utility of ImPACT assessment for postconcussion return-to-play counseling: Psychometric issues. Journal of Clinical and Experimental Neuropsychology. 2012 Mar;34(3):235–42.
Taylor K, Brooks B, Schneider K, Blake T, McKay C, Meeuwisse W, et al. Neurocognitive performance at return to play in elite youth hockey players with sport-related concussion. Br J Sports Med. 2014;48(7):664–4.
Marshall CM, Tran P, Chan N, Dematteo C. The use of an intensive physical exertion test as a final return to play measure in concussed athletes: a prospective cohort. Phys Sports Med. 2018;22(3):1-9.