Here is why I recommend that high-risk, contact-athletes & concussion patients do not overlook fish oil (omega-3 fatty acids).
Omega-3s, athletic performance, brain health, and you.
In this post, we're going to take a pretty in-depth look at fish oil and breakdown the benefits for concussion patients and athletes at higher risk of concussion (e.g., rugby, American football, ice hockey, etc..).
Fish oil is among the ranks of popular supplements like Vitamin D and curcumin, where folks tout incredible benefits for every health condition under the sun.
While I can't say that I consider any one of these supplements to be an all-encompassing panacea, I think they can each play their part in appropriate doses at appropriate times. For example, Vitamin D only really appears to be helpful when there are adequate/optimal levels before a concussion/TBI. Thus, I tend to check an athlete's vitamin D levels before their season gets underway to ensure optimal levels.
Getting back to fish oil, it appears that these friendly omega-3 fatty acids play beneficial roles in concussion prevention and treatment after a concussion. And newer testing allows us to monitor omega-3 levels, just like we could measure your vitamin D.
So, what's the deal with fish oil (EPA/DHA)?
Fish oil (combined EPA/DHA) has researched benefits across many organ systems and health conditions. To keep this (mostly) brief, we're going to look at HOW fish oil works and WHY it is proving awesome in concussion.
Biology throwback.
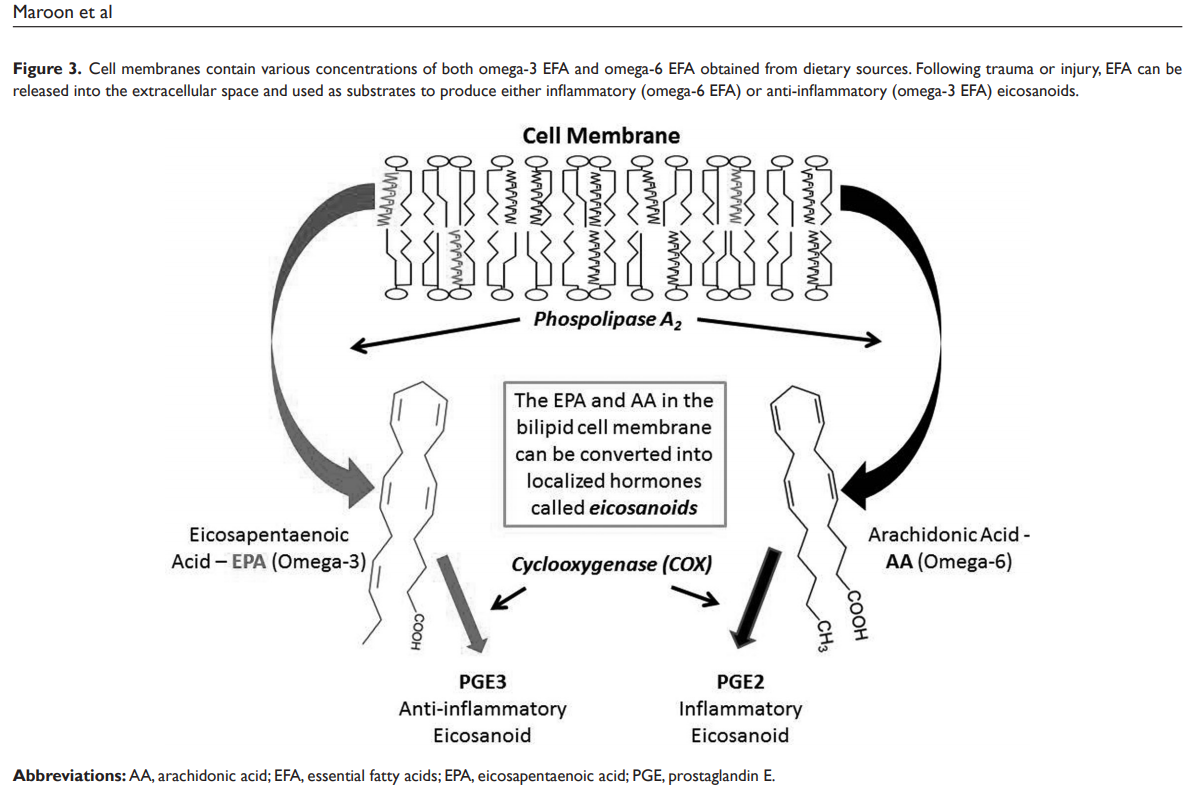
To begin, we've got to take it back to our introductory biology courses. Our body is composed of beautiful organizations of cells, and each cell has a cell membrane - jogging up any memories? Well, your cell membrane is composed of two layers of fats, also called lipids (i.e., phospholipid bilayer). That membrane does more than create an active border for your cell to accept nutrients, remove wastes, respond to hormones, etc...
Think of the membrane as a wall, and the lipids are the bricks that make the wall. If you take away a brick, you can use it to build something else.
While way oversimplified, that is sort of what happens. When your body is dealing with stressors (e.g., inflammation and oxidation), enzymes swoop in to "activate" these lipids ("removing bricks") to regulate the inflammatory and immune responses.
Here you can see the EPA “brick” is an anti-inflammatory omega-3 fatty acid, while the AA “brick” is an inflammatory omega-6 fatty acid.
Our diet & Our biology.
We just recalled that our cells have membranes, and those membranes are primarily lipids. Inside of those membranes, you have different types of lipids. And, the major lipids in the conversation here are:
Linolenic Acid --> Omega-6 fatty acid
Arachidonic Acid --> Omega-6 fatty acid
Alpha-Linoleic Acid --> Omega-3 fatty acid
Eicosapentaenoic Acid (EPA) --> Omega-3 fatty acid
Docosahexaenoic Acid (DHA) --> Omega-3 fatty acid
When your enzymes go to activate lipids to respond to the stressors, they don't discriminate. It's first-come, first-serve, so whichever type of lipid (brick) predominates is more likely to get activated. Well, the bricks that predominate likely correlate strongly with the bricks you eat.
That brings us to the conversation around omega-6 and omega-3 fatty acids. Both of these are essential, meaning our bodies can't make them, and without them, our metabolism is shot - we need to eat these fats to live.
Omega-6 fatty acids are considered more pro-inflammatory; when these bricks are chosen, they create inflammation. And we need this at times - you would never heal a wound without an upregulation in inflammation.
Source: Linus Pauling Institute
Omega-3 fatty acids are considered more anti-inflammatory; when these bricks are chosen, they decrease or regulate inflammation. It should go without saying that this is beneficial in our society obsessed with anti-inflammatory supplements (e.g., curcumin) and over-prescribed anti-inflammatory medications (e.g., NSAIDs).
Source: Linus Pauling Institute. Note: Humans only convert 12% (male) to 30% (female) of ALA to EPA and DHA. The differences between men and women may be due to estrogen.
Source: Linus Pauling Institute
Our search for the perfect supplement might slow down if we figured out our diets first. Remember, we eat the fats (lipids) that create our membranes. And in the US, we tend to eat at a ratio of 15-20 omega-6 fats for every 1 omega-3 fat. That is a ratio heavily tilted in favor of pro-inflammatory lipids. Paleo humans, Greek folks before 1960, and wild animals all have an omega-6:omega-3 ratio closer to 1:1. Hmmm...
Bringing it all together - our bodies are made of cells that have membranes made of fats. Those fats act as inflammation regulators when the body needs to respond to stressors. Omega-6 fats tend to promote inflammation, while omega-3 fats tend to decrease inflammation. Based on our diets in America, we can assume our membranes have 15-20 times more omega-6 fats to choose from than omega-3 fats. In times of stress or injury (e.g., concussion), just by sheer numbers, these omega-6 fats are more likely to be the selected "bricks" when we'd rather omega-3 blocks. A more favorable overall metabolic profile and "injury recovery profile" would include a more optimal omega-3 fatty acid level in our cell membranes.
What can we do with this information?
One way we can make our fats and diets work in our favor as folks recovering from a concussion or athletes looking to minimize concussion damage is to be sure that we have enough "good bricks" in our cells.
An emerging test for this is the Omega-3 Index. I run this test for contact-athletes without injury and concussion patients in the acute and chronic stages because it tells me about their "bricks" - how many omega-6 bricks, omega-3 bricks, and the ratio of omega-3 bricks to all the other bricks (and by "bricks," I mean fatty acids).
These are my personal results from summer 2020.
This test looks at your red blood cells and their membranes. The omega-3 index is the percentage of omega-3 fatty acids compared to all the other lipids in the membrane. Below are the ranges that the research is forming based on improving cardiovascular and neurometabolic health:
<4% Poor
5-8% Okay
8-11% Good ("Optimal")
Here you can see I’m almost in the ideal 8-11% range. If you look above, my total omega-6 to total omega-3 ratio is approximately 3:1. Thus, my omega-3 index would likely be “optimal” if I ate less fried foods and foods with higher omega-6 levels.
Summary: We want 8-11% of all the lipids in your membrane to be omega-3 fatty acids. We want the ratio of omega-6 to omega-3 that we eat to be closer to 2:1 or 1:1 (compared to 15:1). This ensures that oxidation, inflammation, and injury are handled with the right amount of inflammatory and anti-inflammatory lipids.
Omega-3 Index and Athletes
If the standard American eats a diet with a 15:1 ratio of omega-6 to omega-3 (or worse), then we can assume that their omega-3 index is not ideal. But, what about an elite athlete who is at risk of head injury and would acutely benefit from having ideal omega-3 levels?
Well, across the NCAA, the average omega-3 index appears to be "poor" to "okay." In one study of both male and female NCAA athletes, the average omega-3 index was 4.3%. In another study of only NCAA football players, 0% of the athletes had a "good/optimal" omega-3 index. And the more intense and energy-demanding a season is, the more the omega-3 index decreases over the season.
From a performance standpoint, a better omega-3 index is associated with:
Less delayed onset muscle soreness (DOMS)
Less muscle breakdown and inflammation
Better motor control (i.e., mitigated loss of function)
Better reaction times
Better membrane stability (talked about more below with concussions)
So, elite athletes tend to have lower omega-3 index levels and are at risk of lowering their omega-3 index levels throughout their season. This can impair their recovery and performance. If in a contact sport, this places them at greater risk of a more significant head injury due to more pro-inflammatory bricks in their system.
Let's talk more about fish oil in concussion.
A concussion, also called mild traumatic brain injury (mTBI), is a functional and temporary brain injury with physical and metabolic consequences. Physically, your brain cells (neurons) stretch and sheer - not enough to tear, but enough to cause metabolic issues. Metabolically, your neurons leak electrolytes, release excitatory neurotransmitters, and flood with calcium. The calcium flood overwhelms your energy-producing mitochondria, and you're left with a metabolic energy deficit that lasts for 21-30 days in most cases.
Your neurons, just like any other cells, have a membrane. In the brain, 10-20% of all fat is omega-3 fat, and up to 97% of those omega-3 fatty acids are DHA, making DHA a crucial structural component and 100-fold more abundant than EPA in the central nervous system. In animal studies of concussion, we see DHA levels decrease after injury. Animals who were "deplete" (~70%) in DHA had more protein breakdown, cell death, slower motor control recovery, more anxiety, and cognitive deficits than the animals "replete" in DHA.
Most of the nutritional and metabolic data we have on concussion and TBI comes from animal studies, because it would be quite unethical to purposely concuss people. With that, we tend to see that supplemental fish oil:
Maintains overall cellular homeostasis (another throwback biology term)
Stabilizes your genes (i.e., prevents genomic instability)
Improves neuroplasticity by promoting brain-derived neurotrophic factor (BDNF) and neurite outgrowth
Promotes a healthy brain immune response (i.e., clearance of neutrophils)
Reduces overall damage of the injury
Some of the effects above might be explained by having adequate levels before the concussion. When EPA/DHA are supplemented before a concussion we see:
Protection against reduced plasticity by normalizing protein levels in neuronal circuits associated with learning, cognitive processing, synaptic facilitation, neuronal excitability, and locomotor control.
Reduced markers of injury (e.g., Neurofilament Light, NFL) and apoptosis (“programmed cell death”)
Minimizes white matter damage and preservation of nerve coats (i.e., myelin)
Minimizes glutamate excitotoxicity.
Protect against calcium overload & preserves mitochondria function
Bringing it all home.
As humans, we are made up of cells. Each cell has a membrane made of fats (lipids).
Ideally, 8-11% of those fats in your membranes are of the omega-3 variety. In addition to minimizing metabolic disease risk, these levels can improve athletic performance and recovery.
Taking it over to concussion makes sense as your brain is mostly fat. In the brain 10-20% of the fat comes from omega-3 fats, and DHA makes up ~97% of the omega-3 levels in the central nervous system (compared to EPA). Having adequate omega-3 levels before a concussion can reduce the physical and metabolic damage, and supplementing after a concussion can help recover metabolic balance and neurocognitive performance.
This is why I test for omega-3 levels and recommend quality omega-3 supplements for my athletes and concussion patients.
Pretty freaking cool for such a simple thing, huh?
Dr. Mark Heisig is a licensed naturopathic doctor with continuing mTBI education from The American Academy of Neurology (AAN), Complete Concussion. Management (CCMI) and The Carrick Institute. His office is located in Scottsdale, AZ.
References (some may be “duplicate” within this list):
Anzalone, A., Carbuhn, A., Jones, L., Gallop, A., Smith, A., Johnson, P., ... & Oliver, J. M. (2019). The omega-3 index in National Collegiate Athletic Association division I collegiate football athletes. Journal of athletic training, 54(1), 7-11.
Ashbaugh, A., & McGrew, C. (2016). The role of nutritional supplements in sports concussion treatment. Current sports medicine reports, 15(1), 16-19.
Maroon, J. C., LePere, D. B., Blaylock, R. L., & Bost, J. W. (2012). Postconcussion syndrome: a review of pathophysiology and potential nonpharmacological approaches to treatment. The Physician and sportsmedicine, 40(4), 73-87.
Oliver, J. M., Anzalone, A. J., & Turner, S. M. (2018). Protection before impact: the potential neuroprotective role of nutritional supplementation in sports-related head trauma. Sports medicine, 48(1), 39-52.
Pender, S. C., Smith, A. M., Finnoff, J. T., Huston III, J., & Stuart, M. J. (2020). Concussions in Ice Hockey—Moving Toward Objective Diagnoses and Point-of-care Treatment: A Review. Current sports medicine reports, 19(9), 380-386.
Petraglia, A. L., Winkler, E. A., & Bailes, J. E. (2011). Stuck at the bench: Potential natural neuroprotective compounds for concussion. Surgical neurology international, 2.
Ritz, P. P., Rogers, M. B., Zabinsky, J. S., Hedrick, V. E., Rockwell, J. A., Rimer, E. G., ... & Rockwell, M. S. (2020). Dietary and Biological Assessment of the Omega-3 Status of Collegiate Athletes: A Cross-Sectional Analysis. PLoS One, 15(4), e0228834.
von Schacky, C. (2020). Omega-3 index in 2018/19. Proceedings of the Nutrition Society, 1-7.