This is the most common cause of vertigo & how we handle it: BPPV treatment
Quick Summary: BPPV stands for "Benign Paroxysmal Positional Vertigo," the most common cause of vertigo. All of that is a mouthful that states BPPV is a type of vertigo that won't kill you (benign), and sometimes suddenly (paroxysmal) happens when you move your head (positional). It's due to dislodged "crystals" moving through your vestibular canals to create a false sense of motion - spinning. The treatment involves physical repositioning maneuvers to guide the crystals out of the canals and back to their "homes." There's also some exciting research finding a link between healthy vitamin D levels and less recurrence of BPPV. There is a definite relationship between concussion and BPPV due to the nature of head trauma. Additionally, the research is far from certain, though we may see more vertigo/dizziness secondary to COVID. Regardless of risk factors or cause, getting to a qualified healthcare professional for evaluation and treatment can provide relief in as little as 1-2 sessions.
Let's define BPPV.
We already covered this above, but let's really spell it out here.
Benign - Not life-threatening.
Paroxysmal - Sudden and/or intermittent
Positional - Related to the position of your head
Vertigo - A false sensation of body motion (spinning) that lasts 15-30 seconds (up to 60 seconds)
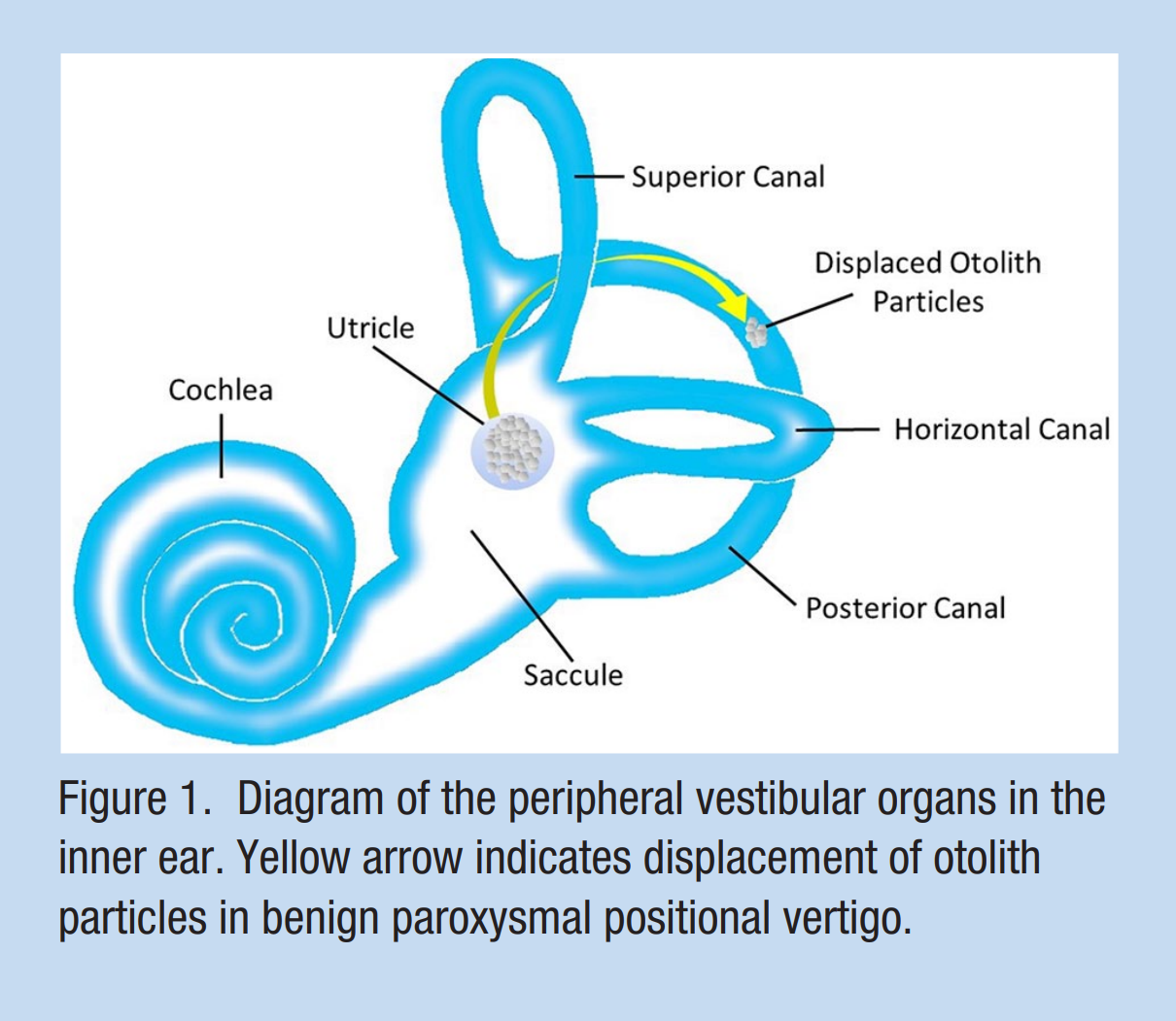
BPPV occurs when an otoconium ("inner ear crystal") breaks free from the otolith and drifts through your semicircular canals. These semicircular canals are what your body uses to detect angular acceleration. So, when that crystal moves fluid through the canals, your brain perceives angular acceleration - even when you're not moving—thus... spins.
From reference #6 below.
This is also why your head position matters. As you move your head in various positions, gravity moves that crystal around, causing the sensation of movement.
Who is most impacted or at risk?
The classically reported risk factors for BPPV are:
Head trauma
Surgery
Inner ear disease
Prolonged head reclining (e.g., dental exams or hair salon)
BPPV tends to impact women 2-3X more often than men, usually women aged 50-60yo.
Other risk factors cited in research include high blood pressure, osteoporosis, sleep disorders, and higher income/city living.
“Keep in mind that these risk factors are not rules written in stone. For example, as a 30yo male, I sustained a significant episode of BPPV involving both my posterior and horizontal canals. - Dr. Mark
What is the treatment for BPPV?
The gold standard is to do a "canalith repositioning maneuver." That's fancy speak for "move your head in ways that put the crystal back in its place."
Depending on your triggering movements and physical exam, we most commonly have to treat for posterior canal or horizontal canal BPPV. These treatments are called the Epley and Lempert ("BBQ Roll") maneuvers. Of your three semicircular canals (posterior, anterior, and horizontal), the posterior canal is the usual culprit (60-90% of cases) for harboring that pesky crystal.
Some at-home maneuvers, like the Modified Somersault for posterior canal BPPV, can be as valuable as the in-office treatments and are even recommended to improve treatment efficacy and reduce the need for multiple office visits.
How often does BPPV come back?
Unfortunately, the risk for recurrence is relatively high at 15-20% annual recurrence. The risk factors for recurrence include:
Female gender
High blood pressure
Diabetes
High cholesterol/lipids
Osteoporosis
Vitamin D deficiency
You'll notice that nutrition, physical activity, and lifestyle can significantly influence four of those factors. For example, physically inactive older women have a 2.6X higher risk for BPPV than regularly active older women. Additionally, a vitamin D level of less than 30 ng/ml can increase your odds of BPPV by 3.8-23 times!
In some cool, repeatable, and growing research, vitamin D supplementation appears to reduce the recurrence of BPPV by 63%. This means that if you've experienced BPPV and don't want another go at it, you should check your vitamin D levels and get them above 30 ng/ml.
You can see an overwhelming agreement among studies that Vitamin D is a favorable intervention for BPPV.
Additionally, classic vestibular rehabilitation like gaze stability, balance, and dynamic movement exercises can get you back to moving worry-free through your world.
Extra credit info
Concussion and BPPV?
Dizziness is a prevalent symptom after a concussion (mTBI). Generally speaking, head trauma is a risk factor for BPPV; still, it's hard to pin all this post-concussion dizziness to BPPV. The prevalence of BPPV ranges from 4.9% to 57% after a concussion. In concussion, we must consider autonomic causes of dizziness (e.g., POTS) and the visual, vestibular, and proprioceptive influences on posture and spatial awareness.
COVID-19 and vertigo/dizziness symptoms?
Now, this is a sidebar that needs more research. But, as a clinician working with long-COVID patients (due to the similarities with PCS), I've noticed that I'm treating more tricky vertigo/dizziness cases, particularly BPPV. So, a quick look at the research and I found the following:
This study evaluated 72 patients with vestibular symptoms after COVID-19 vaccination. The most prevalent diagnoses were somatoform vestibular disorders (e.g., PPPD) and vestibular migraine, with no significant increase in other central or peripheral vestibular syndromes (e.g., BPPV).
This report presents two cases of benign paroxysmal positional vertigo (BPPV) occurring within two weeks of SARS-COVID-19 infection, suggesting a possible connection between COVID-19 and BPPV, with the pathophysiology likely similar to that of other viral infections.
This study evaluated 33 patients with acute vertigo after COVID-19 vaccination, finding that while some had peripheral vestibular dysfunction, others had a central disorder, suggesting the need for further research.
The study found that all eight COVID-19 patients with vertigo had benign paroxysmal positional vertigo (BPPV), and the authors hypothesize that BPPV in COVID-19 infections may be related to drug use, prolonged bed rest, direct damage by viral infection on the peripheral vestibular system, and inflammation.
Together, these studies discuss the possible relationship between COVID-19 and vertigo/BPPV, with some suggesting that the virus can directly damage the peripheral vestibular system and induce BPPV. There are reports of BPPV occurring in COVID-19 patients and in those who have received the COVID-19 vaccine. However, due to the small sample size in some studies, more research is needed to confirm the link between COVID-19 and BPPV/vertigo.
In my practice, we work together to make you make you resilient before or after injuries. I offer in-person care here in Arizona and virtual concussion/PCS programs for folks outside the state and abroad. Over the course of our visits, we dive deeply into autonomic, metabolic, visual/vestibular, cervical, and psychological assessment and screening. By completing this comprehensive assessment in a matter of 2-3 weeks, patients are provided with a comprehensive rehab plan that can shave months off their recovery times.
Request an appointment below for your consultation to begin working together.
References not directly linked:
Gianoli GJ. Post-concussive Dizziness: A Review and Clinical Approach to the Patient. Front Neurol. 2022 Jan 4;12:718318. doi: 10.3389/fneur.2021.718318. PMID: 35058868; PMCID: PMC8764304.
Jeong SH, Lee SU, Kim JS. Prevention of recurrent benign paroxysmal positional vertigo with vitamin D supplementation: a meta-analysis. J Neurol. 2022 Feb;269(2):619-626. doi: 10.1007/s00415-020-09952-8. Epub 2020 Aug 7. PMID: 32767116.
Józefowicz-Korczyńska M, Pajor A, Skóra W. Benign paroxysmal positional vertigo in patients after mild traumatic brain injury. Adv Clin Exp Med. 2018 Oct;27(10):1355-1359. doi: 10.17219/acem/69708. PMID: 30058780.
Kim HJ, Park J, Kim JS. Update on benign paroxysmal positional vertigo. J Neurol. 2021 May;268(5):1995-2000. doi: 10.1007/s00415-020-10314-7. Epub 2020 Nov 24. Erratum in: J Neurol. 2021 Feb 23;: PMID: 33231724; PMCID: PMC7684151.
Reneker JC, Cheruvu VK, Yang J, James MA, Cook CE. Physical examination of dizziness in athletes after a concussion: A descriptive study. Musculoskelet Sci Pract. 2018 Apr;34:8-13. doi: 10.1016/j.msksp.2017.11.012. Epub 2017 Nov 26. PMID: 29197811.
Wang A, Zhou G, Kawai K, O'Brien M, Shearer AE, Brodsky JR. Benign Paroxysmal Positional Vertigo in Children and Adolescents With Concussion. Sports Health. 2021 Jul-Aug;13(4):380-386. doi: 10.1177/1941738120970515. Epub 2021 Feb 2. PMID: 33528343; PMCID: PMC8246417.