Lab Series: What does a lipid panel tell us?
Quick Summary: A lipid panel is widely used conventionally to asses your overall cardiovascular health. The test looks at different lipids (i.e., fats) and proteins in your blood. We need each of these lipids to be healthy and perform optimally. However, too many can be problematic for your cardiovascular and neurological health. And it is far too common in North American/Western societies to find abnormal lipid panels. Let's look at the biomarkers measured, where they come from, and what they mean for your health.
Cholesterol: Friend or foe?
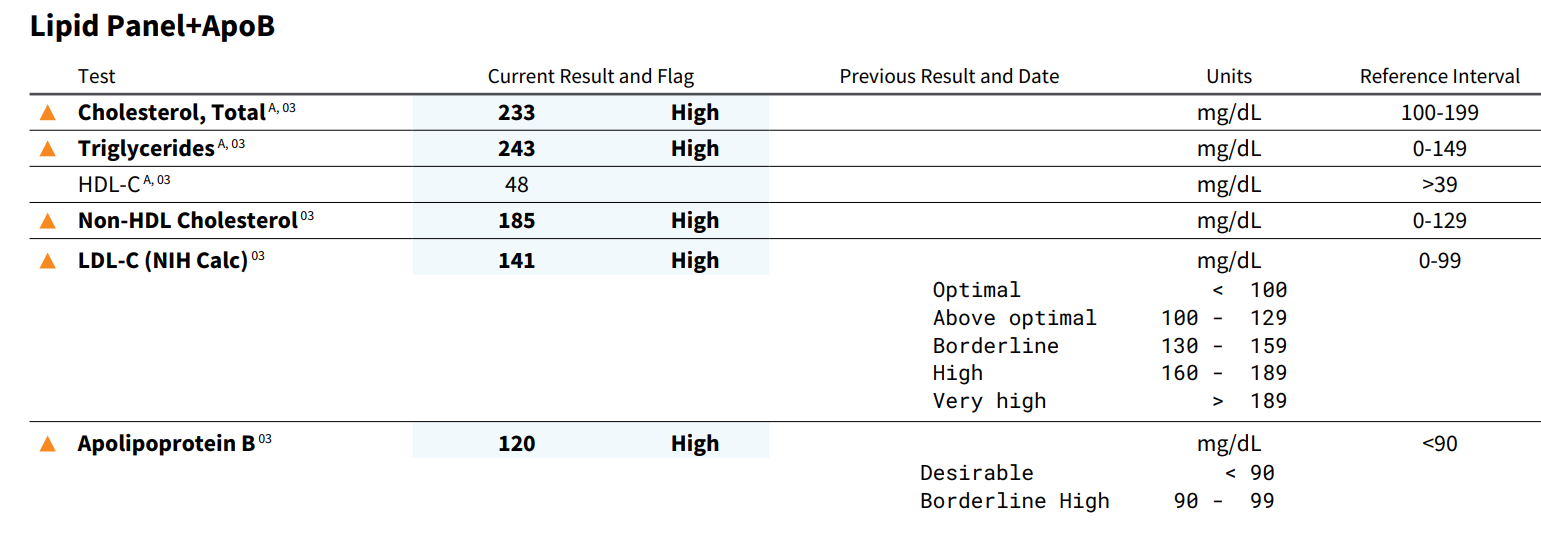
Example of an unfortunately common patient lipid panel.
How about both, and the dose makes the poison? Cholesterol is a steroid molecule produced by the liver and absorbed (or removed) from foods in our diet. We use cholesterol for steroid hormone production (e.g., estrogen and testosterone), bile acid production (e.g., fat digestion), cell membrane stability, and other nifty things.
However, too much specific cholesterol - or cholesterol carrier proteins (e.g., LDL) - correlates with heart disease like stroke, heart attack, coronary artery disease, etc...
Total Cholesterol: We'd like this number below 200 mg/dL. Borderline high cholesterol is between 200-239 mg/dL, and high cholesterol is >240 mg/dL.
Depending on lifestyle factors (e.g., diet, alcohol, smoking) and family history, we will make treatment recommendations that range from only lifestyle modifications to lifestyle modifications + medication (e.g., statin or PCSK9 inhibitors).
"Good vs. Bad" Cholesterol.
Maybe you've heard of "good cholesterol" and "bad cholesterol." What that's referring to is the density of proteins (i.e., lipoproteins) used to carry the protein.
High-Density Lipoprotein (HDL; "Good") We like to see HDL >40 mg/DL. HDL gets its "good" designation because it's involved in taking up cholesterol from the blood and moving it around. Generally, more is better.
Low-Density Lipoprotein (LDL; "Bad") We like to see LDL <99 mg/dL. LDL gets its "bad" designation because it's associated with depositing cholesterol throughout the cardiovascular system. Too much LDL (paired with other factors like hypertension) can increase your risk of clotting/stroke and cardiovascular events.
Triglycerides: What are these?
Triglycerides are not steroids like cholesterol; they are fatty acids. More specifically, three fatty acids are attached to a glycerol molecule to make a triglyceride. Insulin dysregulation, blood sugar mismanagement, and diets high in refined carbohydrates will increase triglycerides. We like to see these buggers <149 mg/dL.
Newer tests: ApoB and Lp(a).
We can use ApoB as an additional biomarker to assess CVD risk.
It should be becoming more evident now that it's not as simple as "high cholesterol bad" and "low cholesterol good." We have to look at our total cholesterol in the context of HDL and LDL levels. Further down the rabbit hole, we can look at other lipoproteins involved in cholesterol metabolism.
Apoprotein B is the main protein found in LDL and the primary protein receptor to take up LDL. Thus, high levels of Apo B tend to infer high levels of LDL activity. While ApoB is not necessarily first-line at this time, it helps predict cardiovascular disease. And because it's modifiable, we can track it to monitor treatment progress.
Lipoprotein a ("little A") is similar to LDL in that it can build up in the walls of your blood vessels, restricting blood flow and increasing stroke risk. Lp(a) can also promote inflammation, increase clotting risk, and narrow/stiffen your heart valves. High levels of Lp(a) correlate with cardiovascular risk.
Wrap-up
While it could be better, there is a tool called the ASCVD Risk Calculator. You punch in your age, blood pressure, lipid measures, and lifestyle factors to get your lifetime and 10-year cardiovascular risk. It could be better because it can over- and underestimate risk depending on various factors (e.g., age, sex, genetics, exercise status, etc...).
However, it's a great starting point to empower a conversation with your provider:
What is your lifetime risk of CVD?
If you're old enough, what's your 10-year risk?
Are there lifestyle factors that could improve this risk?
Are there indicated medications?
Could your doctor provide nutritional support to minimize medication side-effects (e.g., myalgia or CoQ10 depletion)?
Etc...
In my practice, we work together to make you make you resilient before or after injuries. I offer in-person care here in Arizona and virtual concussion/PCS programs for folks outside the state and abroad. Over the course of three visits, we dive deeply into autonomic, metabolic, visual/vestibular, cervical, and psychological assessment and screening. By completing this comprehensive assessment in a matter of 2-3 weeks, patients are provided with a comprehensive rehab plan that can shave months off their recovery times.
Request an appointment below for your consultation to begin working together.