Your brain scrubs itself clean while you sleep. Has your concussion messed this cleaning (and your sleep) up?
Article teaser and punchline: We have some reason to believe that concussion may be correlated with sleep disturbance and glymphatic dysfunction. And both of these issues (i.e., sleep and glymphatic dysfunction) may lead to the persistence of concussion symptoms (e.g., postconcussive headache) and increased vulnerability to neurodegeneration. By addressing sleep and our glymphatic system, we may be able to improve concussion recovery.
Sleep disturbance after a concussion.
After a concussion, are your headaches, memory problems, anxiety, and other mood disturbances related to sleep or independent symptoms? It turns out that this might be a "chicken or egg?" type of situation because of the well-documented, two-way relationship between our sleep and our physical/mental/emotional health.
Research tells us that roughly 30-70% of folks will deal with persistent sleep issues after a concussion. The majority of these folks (~30-60%) will have trouble sleeping at night, leaving them sleepy during the day. In contrast, the other chunk of folks (~30%) will be excessively tired all the time. We also see that folks recovering from a concussion have more NREM stages and fewer REM stages of sleep.
Having sleep troubles like this in either direction (sleepy vs. can't sleep) could be due to impairment in your brain's standard homeostatic mechanisms:
Glutamate metabolism
Maintenance of cerebral temperature
Maintenance of cerebral glycogen storage
Excessive pro-inflammatory cytokines (e.g., IL-1beta, IL-6, and TNF-alpha)
Dysregulation at the hypothalamus (e.g., orexin, GABA, histamine), pineal gland (e.g., melatonin), brainstem (e.g., norepinephrine, serotonin), and cortex (e.g., glutamate).
Disruption of these functions leads to alterations in your wakefulness and sleepiness. Well, as you'll soon read, these alterations in sleep may partake in a bidirectional relationship with glymphatic dysfunction.
What is the glymphatic system?
"The glymphatic system is a recently discovered macroscopic waste clearance system that utilizes a unique system of perivascular channels, formed by astroglial cells, to promote efficient elimination of soluble proteins and metabolites from the central nervous system. Besides waste elimination, the glymphatic system may also function to help distribute non-waste compounds, such as glucose, lipids, amino acids, and neurotransmitters related to volume transmission, in the brain." - The Glymphatic System: A Beginner's Guide
In people's terms: The glymphatic system helps your brain to "bring in the groceries" (e.g., glucose, lipids, proteins) and "take out the trash" (e.g., tau, amyloid).
A vital feature of this system is that it's thought to be most active during sleep and suppressed while you're awake.
Concussion, sleep, and glymphatic dysfunction.
Here's where it all comes together. Your glymphatic system may be one of the links between concussion and persistent symptoms. This likely happens in two ways:
Directly: Concussion may slow cellular waste clearance via the glymphatic system by affecting your glymphatic system protein channel levels (i.e., decreasing AQP4).
Indirectly: Concussion disrupts normal sleep phases. Sleep is when the glymphatic system is most active. By disrupting sleep, a concussion may disturb the normal glymphatic clearance of wastes.
When normal, nightly clearance of waste does not occur, we risk accumulating a build-up of neuropeptides and cellular waste that can contribute to persistent inflammation and symptoms. For example, postconcussive headaches and migraines may be (in part) dependent on the release of the neuropeptide, calcitonin gene-related peptide (CGRP). With the improper glymphatic clearance of CGRP, there may be a build-up of this peptide that perpetuates headache.
Are there any medicines for this problem?
Researchers have found that your glymphatic system is regulated, partly, by central sympathetic ("fight or flight") tone.
In pharmacological (drug) studies with rodents and humans, blocking specific sympathetic adrenaline receptors has improved glymphatic flow and decreased post-traumatic headache pain/frequency. Other more integrative methods like postural adjustment, sleep hygiene, and breathwork are also being researched. All of these modalities need more research.
What can you do to improve this from home?
While we don't have any proven and validated methods at this time, there's no harm in improving your sleep hygiene, ensuring adequate hydration, and taking some time to breathe.
Breathing
Our sympathetic nervous system is part of the regulation of our glymphatic system and was the target of pharmacological treatment. Well, our breathing is a simple way to access and regulate our sympathetic and parasympathetic nervous systems. Doing so can also improve our sleep, and provide a little pump for our brains (see video). You can see that when our hearts beat and we breathe, our brains move and can pump fluid around.
For my patients, I recommend folks using Xhalr or the breathing pacers in the Calm App.
5 second inhale through the nose
5 second exhale through the nose
No holding the breath.
Perform for 10-20min at a time.
This 5:5 breathing slows your breath down to 6 breaths per minute which improves your heart rate variability (HRV) and kicks off other "calming" effects in your brain and body to counteract sympathetic ("fight or flight") overactivity.
Sleep Hygiene
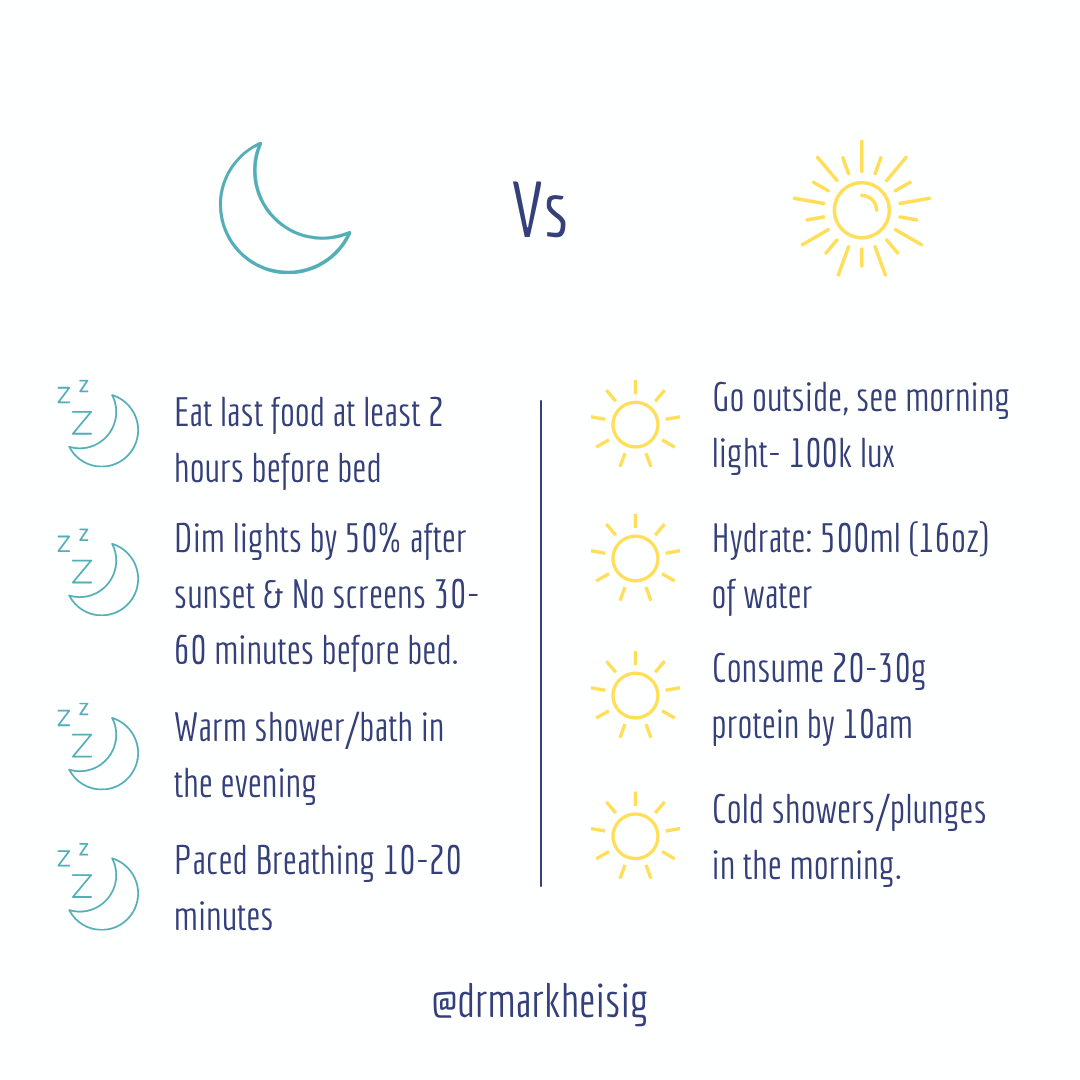
We know that concussion disrupts your sleep phases, and we also know that sleep medications don't improve those sleep phases. While medications may improve sleep quantity, they do not enhance the quality of sleep. Sleep hygiene is a great way to improve the quality of your sleep - and it starts in the morning.
Light is one of the main drivers of your circadian rhythm because light helps us differentiate day from night (i.e., daytime is bright, nighttime is dark). Stepping outside in the morning (before 10 am), no matter how you slept the night before, and getting sunshine in your system acts as a "timestamp" for your brain and body to announce, "it's morning!" On the flipside, making things in your home dim and dark after sunset (or in higher latitudes during the winter months, around 7-8 pm) can help signal to your body, "it's nighttime!" For more on this check out “Why we Sleep” by Dr. Matthew Walker.
Hydration
If I had a nickel for every patient that I saw with concussion/PCS who was not drinking enough water, I still wouldn't come close to paying off my student loans (but I'd have a lot of nickels). Before we even get into glymphatic function, let's talk about hydration in concussion.
When we dehydrate healthy, "non-concussed" folks - they feel and perform concussed. Let me repeat that: dehydrating healthy folks without a concussion makes them feel and function like they have a concussion.
PMID: 17597946
With the whole purpose of the glymphatic system being the nightly flushing and movement of fluid, we want folks to be aiming for 2-3L of water (or non-diuretic tea) consumption every day. That's 68-100oz of water or non-diuretic tea each day. Doing so should make you 1) have to pee a bit more often, and 2) your pee should be a light to very faint yellow color when you go.
Keep in mind that these were not an exhaustive list of recommendations. We also have to consider your cranial structure, cervical lymph drainage, respiratory mechanics, etc, etc, etc…
For more specific help with your post-concussion sleep troubles, headaches, brain fog, dizziness, balance troubles, etc... schedule a consultation below.
Glymphatic References:
Jessen, N. A., Munk, A. S. F., Lundgaard, I., & Nedergaard, M. (2015). The glymphatic system: a beginner’s guide. Neurochemical research, 40(12), 2583-2599.
Piantino, J. A., Iliff, J. J., & Lim, M. M. (2021). The bidirectional link between sleep disturbances and traumatic brain injury symptoms: A role for glymphatic dysfunction?. Biological Psychiatry.