Why can't you sleep with a concussion?
Sleep is important.
You know it and can feel it every night you don't get quality sleep.
Research shows that 30-60% (some even says 70%..) of TBI cases will go on to have some sort of sleep disturbance. And sleep disturbance tends to be more common in mTBI (concussion) than it does in more severe types of brain injury.
With sleep trouble being that common, we should have a good idea about what's going on, right? Well... Not really.
"The relationship between concussion and sleep disturbance is not well understood and sleep disturbance is one of the least studied postconcussion symptoms [4]. It has been suggested that many clinicians assume that sleep disturbance holds little consequence for recovery and will decrease as the other symptoms of concussion resolve [4–6]. There is limited literature on the factors that might predispose an individual suffering from a brain injury to sleep disturbance [5]."
What do we think we know at this point?
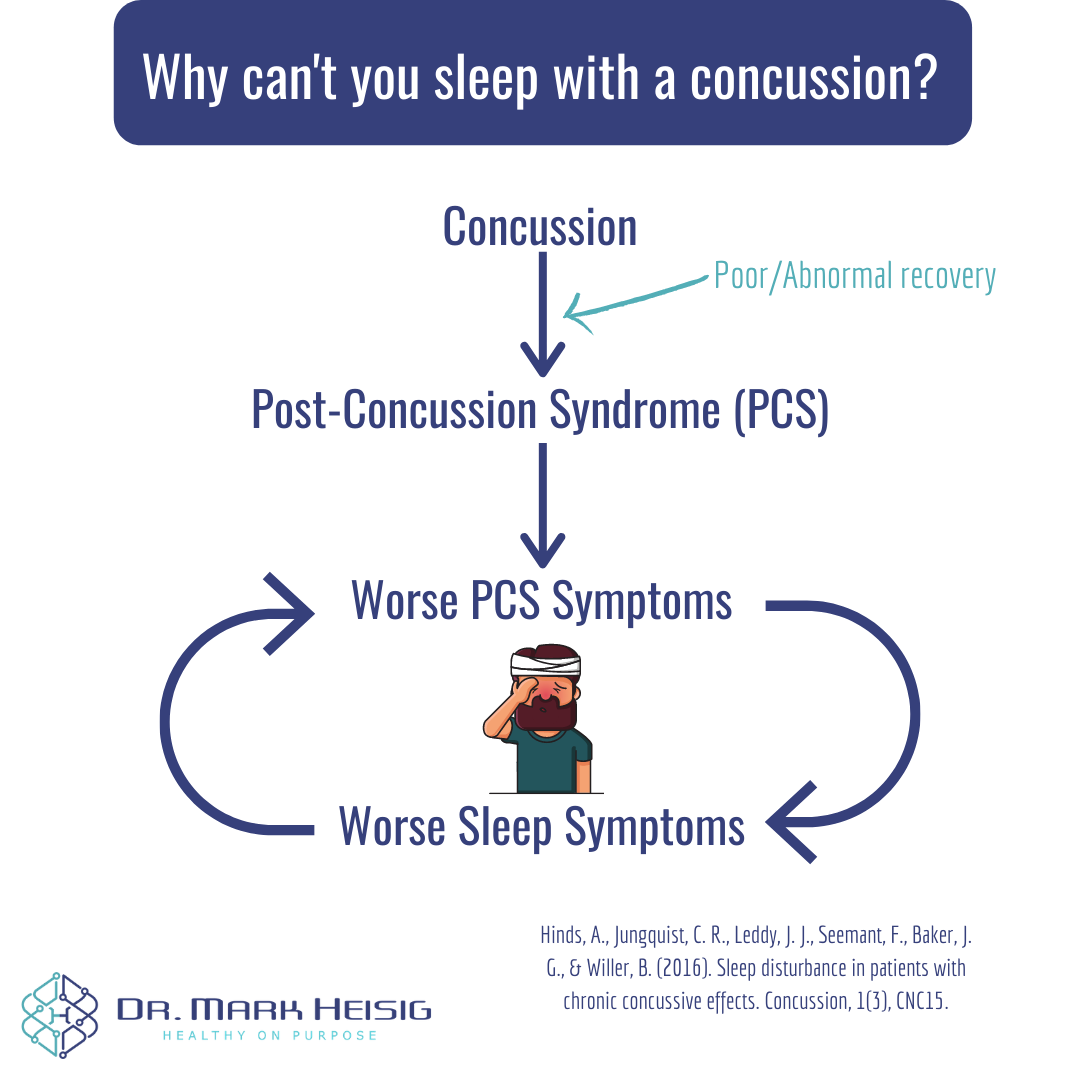
We know that concussion leads to physical, cognitive, emotional, and sleep symptoms.
We think that these other symptoms can impact sleep. For example, we know that people in pain don't sleep as well as people not in pain. So, if you have pain after your concussion, it can be assumed that this pain may be interfering with your sleep.
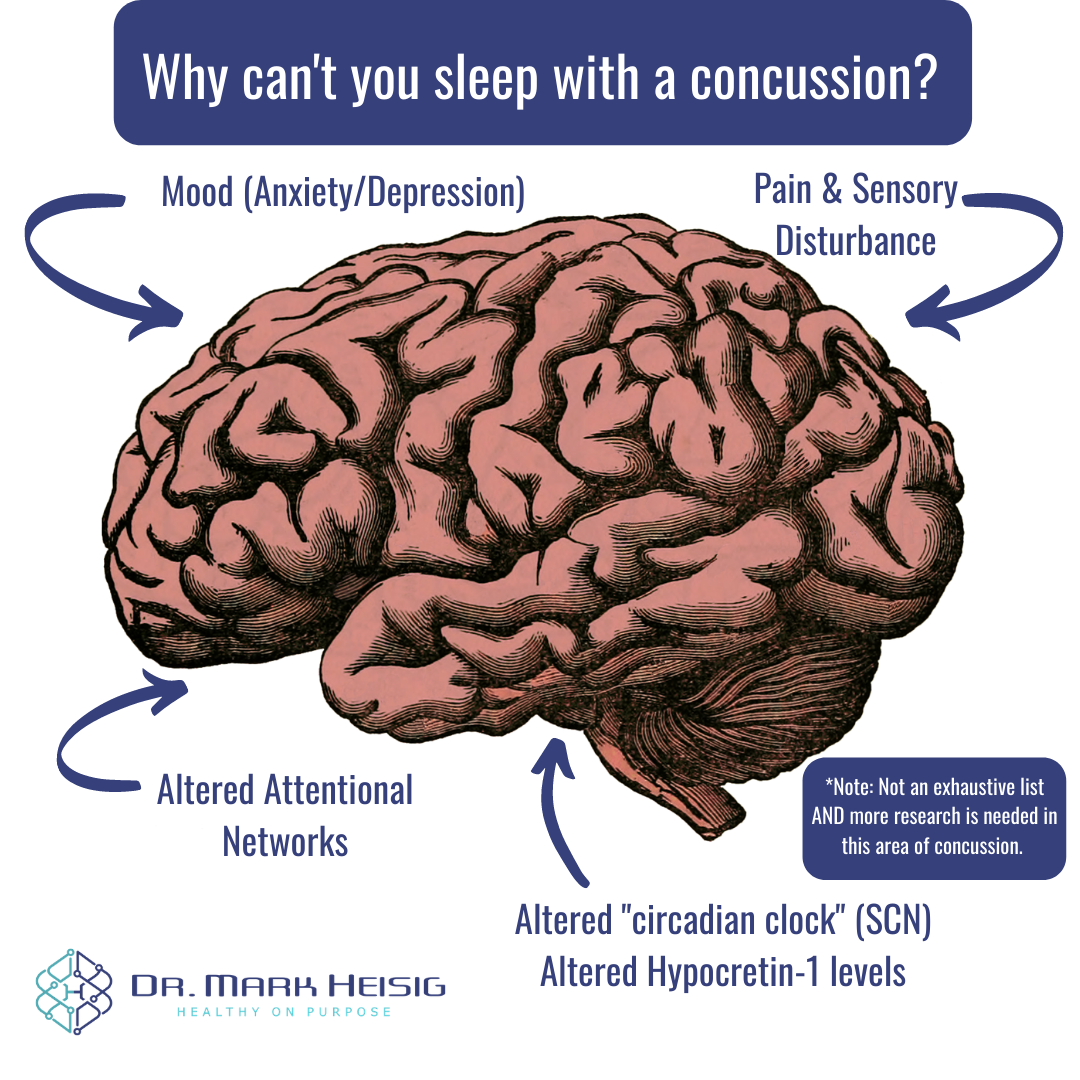
Additionally, we also think about some other things when it comes to TBI and sleep disturbance:
Sleep trouble may be related to alterations in attentional, arousal, and sleep initiation networks ("go figure..." on that last one, right?).
Following TBI we see decreased levels of Hypocretin-1 (Orexin A). This is a neuropeptide that is also low in conditions like narcolepsy.
Additionally, there have been documented changes in the hypothalamus. The hypothalamus houses your "circadian clock" (also known as the suprachiasmatic nucleus; SCN). Altered SCN function will alter your normal wake/sleep cycle.
We also tend to see sleep disturbance more often in cases with anxiety and/or depression involved.
What can be done about it?
If you have worked with me, or follow me on social media in any capacity, then you can guess what's coming up. In case you're not familiar with my practice or my style, you'll learn in a second that movement is a key to optimal health, both in prevention and treatment.
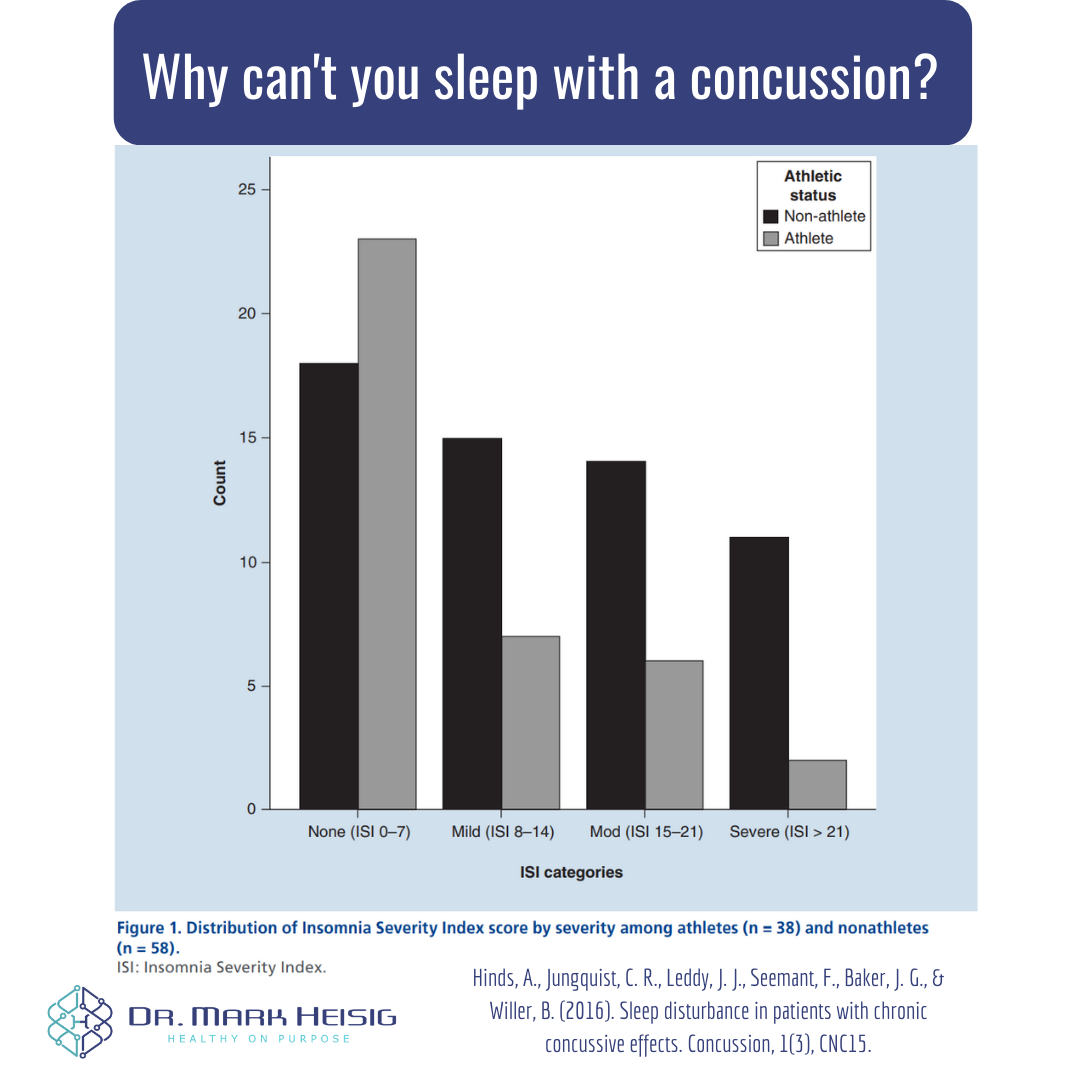
Here's a great example of this. Athletes who sustained a concussion in this study, compared to non-athletes, had less sleep disturbance.
This difference between athletes and non-athletes was attributed to athletes having greater levels of fitness and parasympathetic tone. This increased parasympathetic ("rest and digest") activity helped athletes to do just that - rest.
Always start concussion rehab with subthreshold exercise.
Though sleep disturbance can also be found in cervical and visual/vestibular-driven concussion symptoms, it's always a good idea to rule out a physiologic (blood flow) cause of symptoms AND to improve parasympathetic tone with exercise.
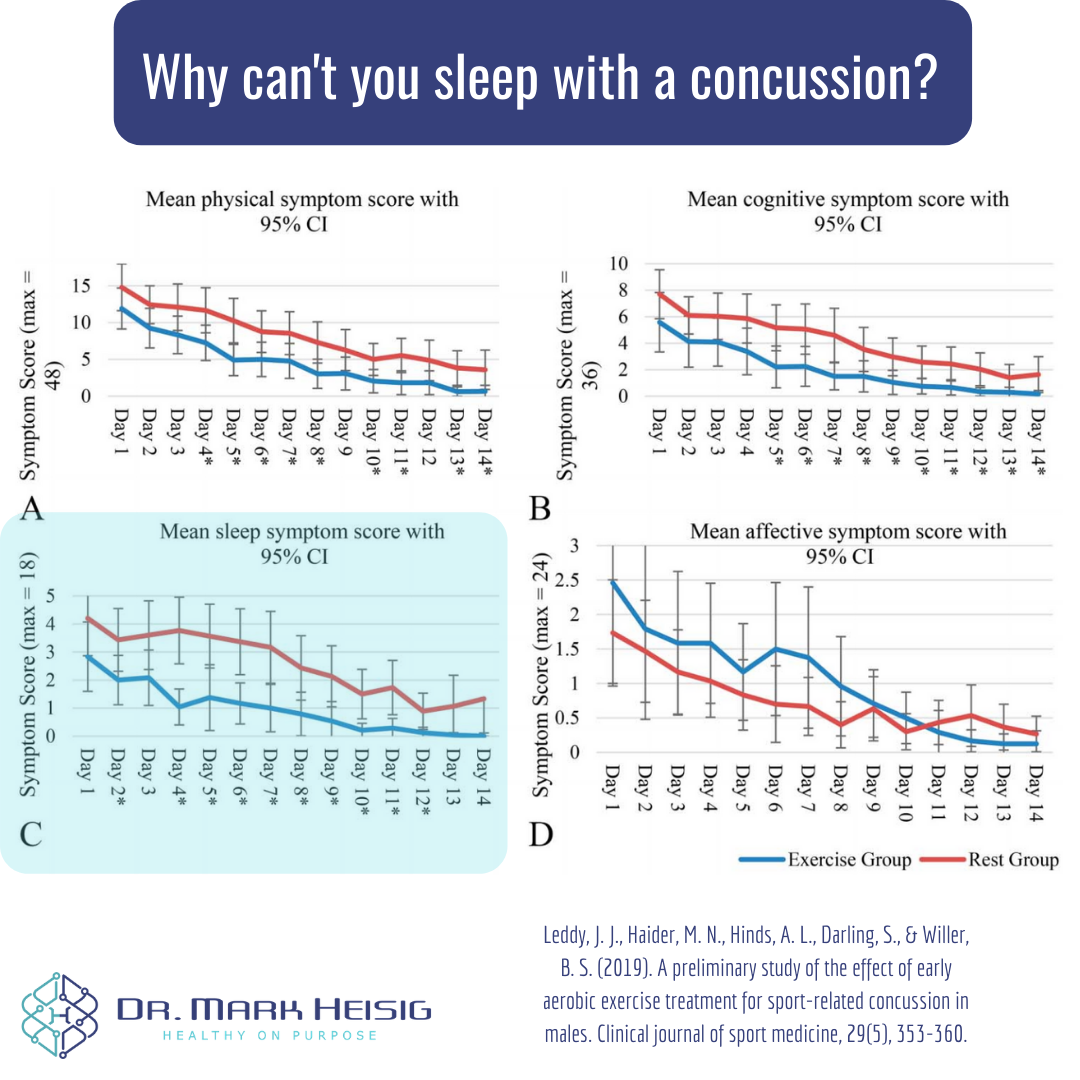
Finding your specific exercise threshold can be completed in-office with a simple treadmill test, The Buffalo Concussion Treadmill Test (BCTT). For an example of how this plays out, this study of exercise in young men found that they recovered from their concussions in about 9 days with sleep symptoms improving first.
Big option #2: Paced Breathing
Paced breathing is exactly what it sounds like - breathing for a specific rhythm and pace.
The research finds that breathing around 6 breaths per minute helps to boost our “coherence.” Simply put, it means that we improve our parasympathetic tone and balance our autonomics. Paired with aerobic exercise, this is an easy way to stack therapies in your favor.
My favorite ways to do this:
Breathe at 6 breaths/min for 5min 2-3 times a day. Always perform 5-10min before bed.
Free option: I use and recommend Xhalr. Set the settings to 5 sec inhale, 5 sec exhale, and 0 sec holding. Simply get set up in a respectable upright, or comfortable lying down position and follow the pacer for 5-10min.
Paid option (not affiliated with me): I recommend patients use Inner Balance by Heart Math. This device measures real-time HRV and allows you to track and train your coherence. This also allows you to “level up” and get more specific and “advanced” in your parasympathetic training.
I usually recommend Inner Balance for patients dealing with stress, anxiety, depression WITH THE CAVEAT and a conversation around the acknowledgement as to whether too much data will simply add to their mental health concerns. There definitely is a line we can cross when it comes to data and biometrics - we can feed our anxiety or depression by worrying about perfect or imperfect HRV numbers. Often just using the free Xhalr website is more than perfect for folks!
Outside of exercise and paced breathing, consider your sleep habits.
Also known as sleep hygiene, your behaviors and rituals around sleep matter A LOT.
Here is a high-yield routine you can adopt from Coach Craig Ballantyne:
10 hours before bed – No more caffeine.
3 hours before bed – No more food or alcohol.
2 hours before bed – No more work.
1 hour before bed – No more screen time (turn off all phones, TVs and computers).
0 – The number of times you will hit the snooze button in the morning.
For more information on sleep:
A nerdy review on sleep, food, supplements, and athletic performance.
A deeper look at sleep hygiene and optimizing your sleep routine.
How you can access cutting-edge concussion care.
At my office in Arizona, I have recently launched a VIP Concussion & Brain Performance Package. This package has two main goals:
Make integrative and comprehensive concussion care affordable and accessible.
Provide athletic and brain performance exercises to optimize life, work, and sport performance while minimizing risk of injury.
Dr. Mark Heisig is a licensed naturopathic doctor with continuing mTBI education from The American Academy of Neurology (AAN), Complete Concussion. Management (CCMI) and The Carrick Institute. His office is located in Scottsdale, AZ.
References:
Hinds, A., Jungquist, C. R., Leddy, J. J., Seemant, F., Baker, J. G., & Willer, B. (2016). Sleep disturbance in patients with chronic concussive effects. Concussion, 1(3), CNC15.
Lavigne, G., Khoury, S., Chauny, J. M., & Desautels, A. (2015). Pain and sleep in post-concussion/mild traumatic brain injury. Pain, 156, S75-S85.
Leddy, J. J., Haider, M. N., Hinds, A. L., Darling, S., & Willer, B. S. (2019). A preliminary study of the effect of early aerobic exercise treatment for sport-related concussion in males. Clinical journal of sport medicine, 29(5), 353-360.
Wiseman-Hakes, C., Gosselin, N., Sharma, B., Langer, L., & Gagnon, I. (2019). A longitudinal investigation of sleep and daytime wakefulness in children and youth with concussion. ASN neuro, 11, 1759091418822405.