Prevention before impact - How to minimize your risk of damage following a mild traumatic brain injury (mTBI).
Concussions happen. The more competitive an athlete is, the less likely they are to report it and play through it. With growing concerns around Chronic Traumatic Encephalopathy (CTE), and the life-threatening problem of Second-Impact Syndrome (very rare), we really don't want athletes playing through concussions.
In this article, we're going to look at:
Understanding nutritional strategies to minimize concussion damage
The 5 metabolic strategies for concussion prevention - in detail.
The bullet-point summary of metabolic concussion prevention.
Feel free to jump to the part of the article that you're most interested in!
The Numbers.
Concussion (also called mild traumatic brain injury; mTBI) is a relatively common injury in contact sports.
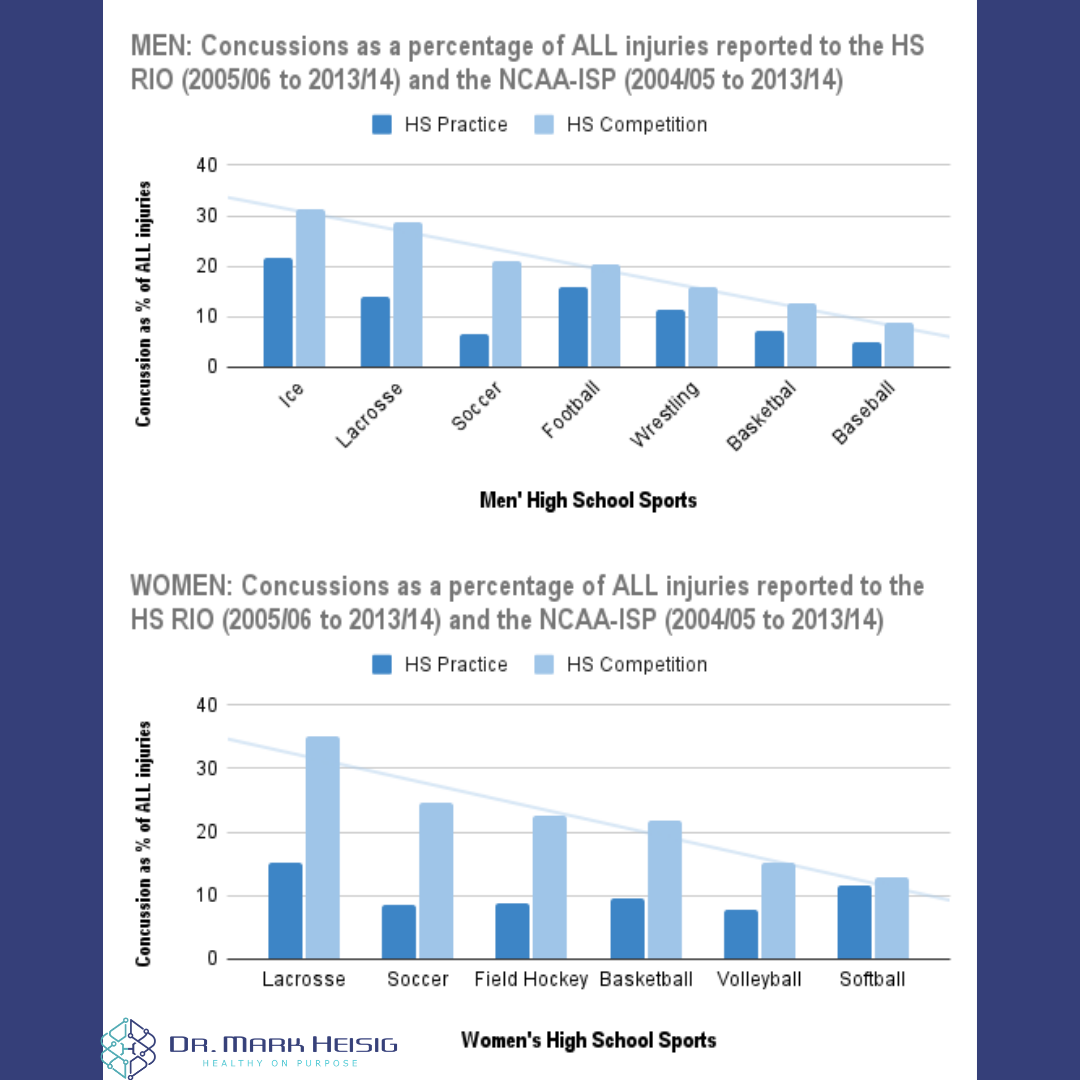
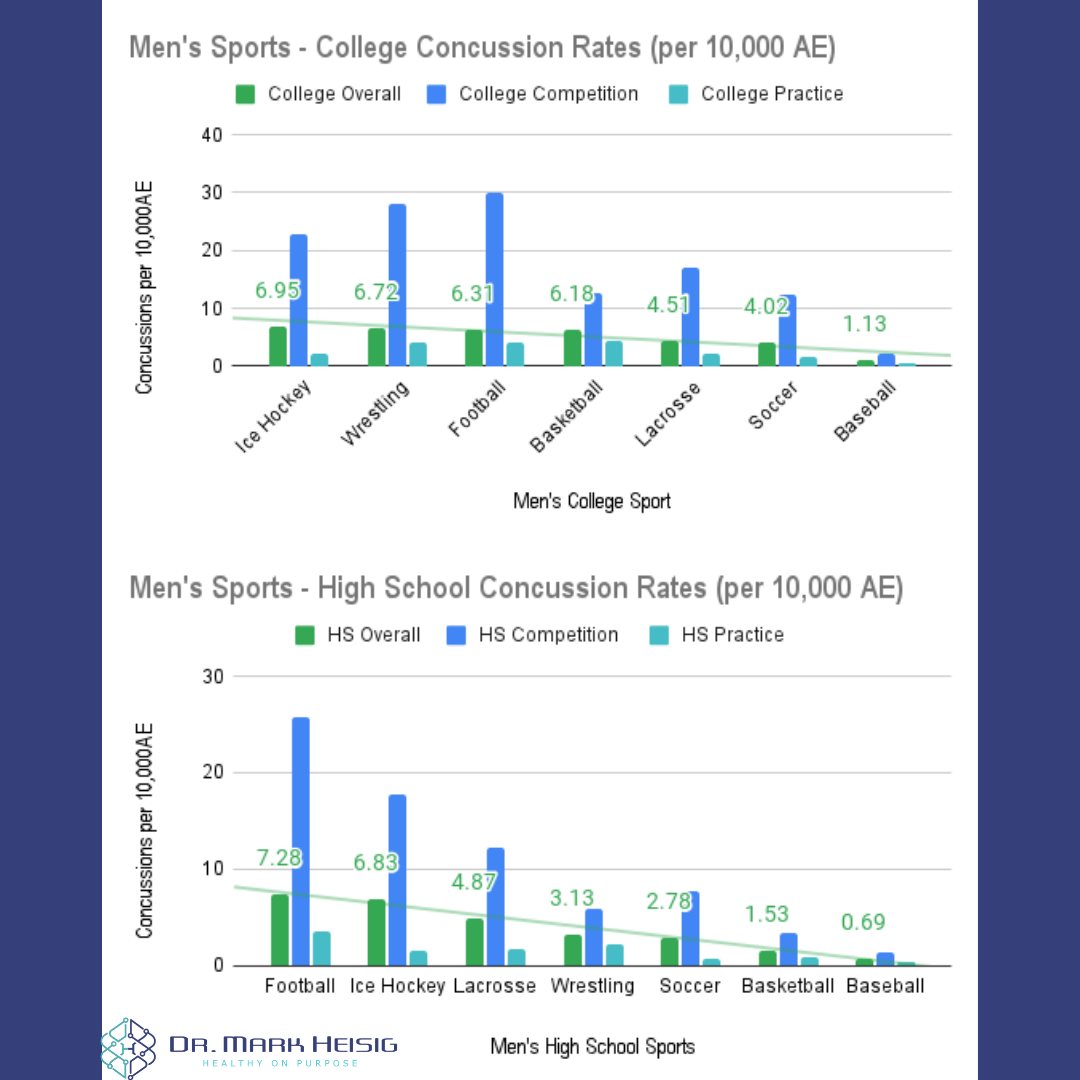
Across men's high school injuries, concussions make up 8.8% to 31.4% of all competition injuries across various sports.
Across women's high school injuries, concussions make up 12.8% to 35% of all competition injuries across various sports.
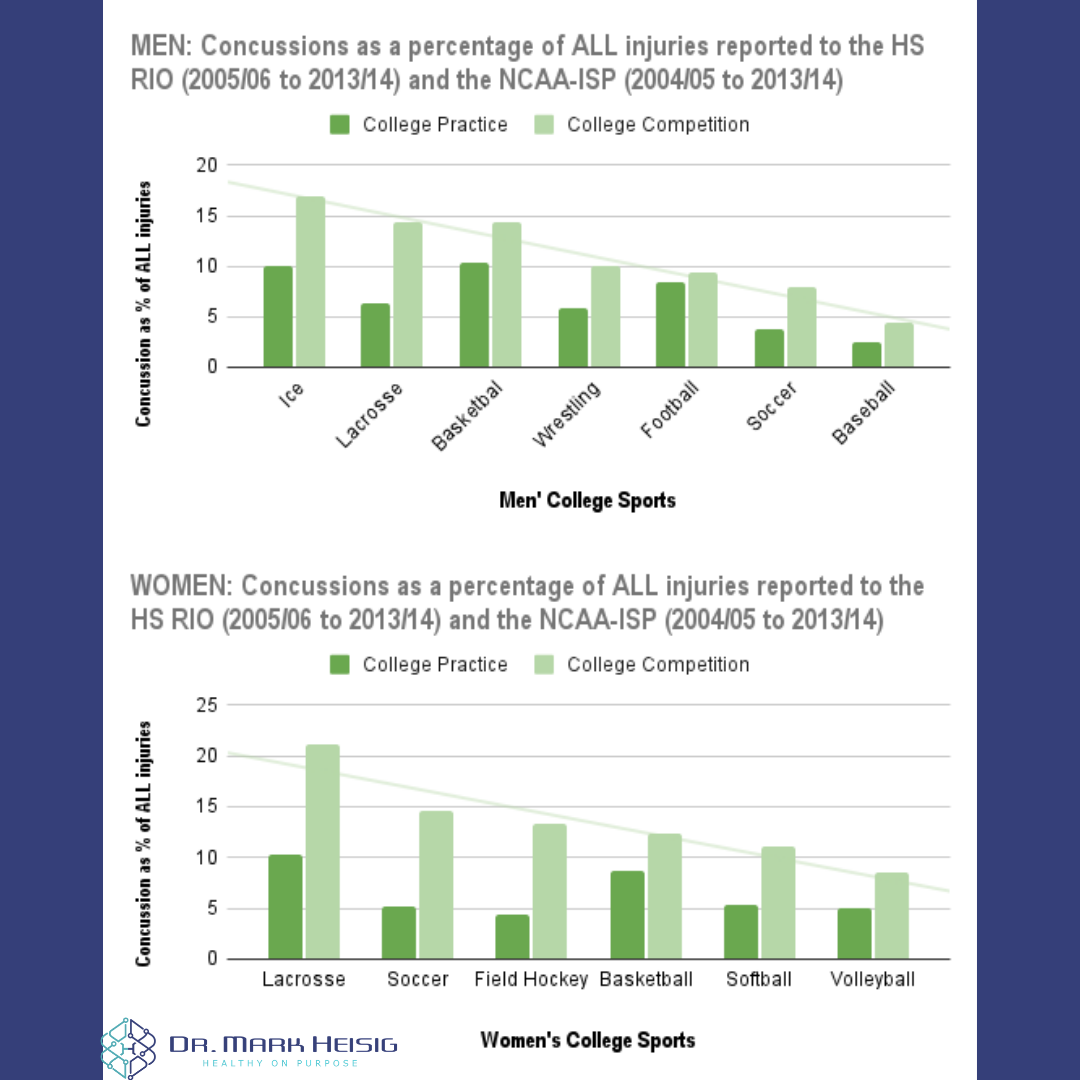
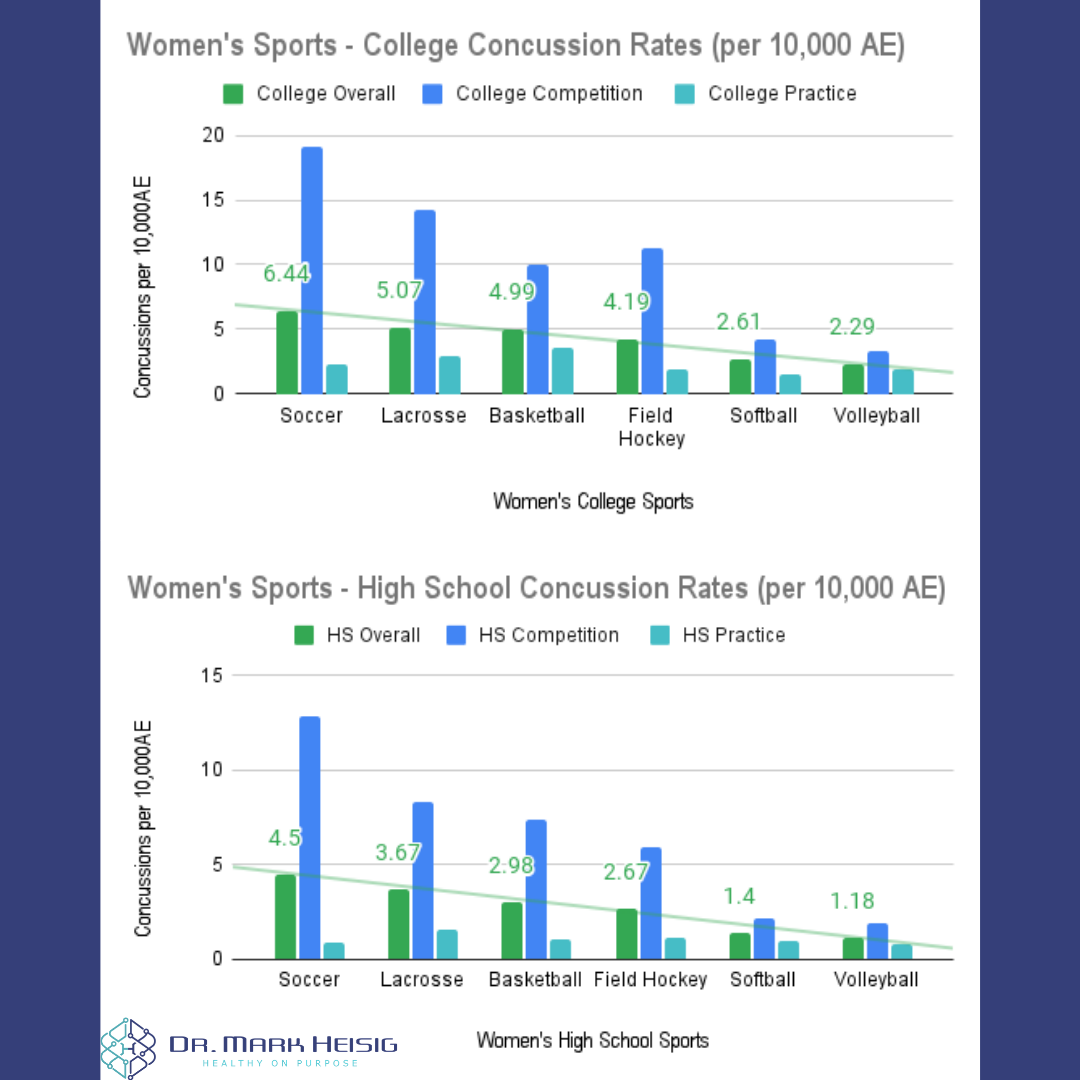
Across men's college injuries, concussions make up 4.4% to 17% of all competition injuries across various sports.
Across women's college injuries, concussions make up 8.5% to 21.2% of all competition injuries across various sports.
At the professional level, "The National Football League (NFL) reported 224 concussions in 2019 and the National Hockey League (NHL) reported a mean of 71.2 to 74.3 concussions per season between 1997 and 2010, although these are likely underestimates." - PMID: 33627496
And, guess what? Research estimates that approximately 50% of sports-related concussions go unreported.
Unreported Concussions.
We just stated that ~50% of sports-related concussions go unreported. Why?
These answers come from a survey of youth athletes:
A significant factor across sexes and ages? Competitiveness.
Researchers can quantify an athlete's level of competitiveness, and what we find is that as competitiveness goes UP, concussion reporting goes DOWN across all ages, genders, and sports.
Simply put, the extrinsic reward of winning is more important to a competitive athlete than their safety and health.
That brings us to the main point of this article.
Concussion prevention: Metabolic Strategies.
Generally speaking, in high school and college sports, concussion makes up roughly 1 in 10 to 1 in 3 of all injuries. And 50% of those concussions go unreported.
We can't stop concussions from happening. No matter the rule changes or education, athletes will still collide, bump, trip, run into equipment, etc... Both on purpose and accidentally. That's just sport.
And we cannot overlook the physical, social, and mental/emotional benefits of sport:
"Being active in sports is one way to maintain a physically fit, healthy lifestyle. In addition to helping maintain a healthy weight, sports participation can increase strength, endurance, and flexibility. Regular physical activity has also been shown to improve psychological well-being, increase self-esteem, reduce depression and anxiety, and improve academic performance." - PMID: 33187601
Not to trigger any non-athletes, but the research generally shows that athletes are better students and people later in the real world than folks who didn't participate in sport. (I'm sure that there's good news for folks in orchestra/band, theatre, etc.., as well. I don't live in that world.)
So, how do we keep our athletes competing and healthy while acknowledging this concussion issue?
One (and not the only) way is to proactively support brain metabolism with nutritional strategies that will improve athletic performance and minimize any metabolic damage of concussion (both reported and unreported).
After a concussion, there is functional stretching and shearing of neurons, excitotoxicity and inflammation, and a blood flow and energy deficit that lasts ~30 days.
If the athlete is going to recovery as quickly as possible, we want to:
Minimize the energy deficit
Support neurons that the concussion stretched
Regulate the inflammation and excitotoxicity.
5 strategies for metabolic concussion prevention.
These are based on the idea that we want to enter our (potential) injury as strong and robust as we can be.
It's easy to knock down an old, dry, and dead tree. It's hard to knock down a vibrant, fed, and hydrated tree. Let's be a vibrant, fed, and hydrated tree, eh?
Let's look at 2 dietary strategies and 3 supplements that I like for nearly all athletes.
1. Aim for a Mediterranean/Plant-Heavy Diet (Note: Keto/Paleo diets, appropriately done, are plant-heavy).
This is just a blanket way to say, "Eat a diet with lean protein, healthy fats, minimally processed carbs, fruits, veggies, and enjoy the little things (e.g., sweets) from time to time." Who's going to complain about that?
The way that I recommend folks get set up with a "Mediterranean Diet" is to head to Precision Nutrition and use their Macronutrient Calculator to build your personalized guide for free. Super useful.
On a molecular level, the Mediterranean Diet increases insulin sensitivity, decreases oxidative stress & inflammation, increases genomic stability (e.g., DNA), increases cellular resistance to stress, and way more. The Mediterranean Diet is one of the most studied, medically validated "diets" to date. These are qualities that support our goals of supporting neuronal structure, regulating inflammation and excitotoxicity, and providing steady energy (e.g., stable insulin/blood sugar).
2. Be aware of your dietary triggers. Also be aware, that you may not have any.
There are food allergies (IgE) that are deadly. These are not those "triggers." What I'm referring to are food intolerances (IgG).
IgE refers to a class of antibodies that can push your immune system so hard that you may experience anaphylaxis - the same reason folks with IgE allergies carry an epi-pen around.
IgG refers to a class of antibodies that will push you immune system at the pace of a slow burn. IgE causes throat swelling, hives, and symptoms within seconds to minutes. IgG causes constipation, diarrhea, skin rashes, acne, brain fog, etc... over days to weeks.
There are common food groups: dairy, gluten, soy, nightshades, etc... that can "irritate" folks. And we see this as an excessive IgG response to specific foods when we perform an IgG Food Intolerance blood lab. Here's an example of what we'll see:
Athlete is sensitive to dairy and doesn't know it. Athlete also has rashes near sweaty equipment areas, bloats with their post-workout shakes, and farts sulfur that could compete with Yellowstone's Old Faithful.
Athlete has a dairy response that takes ~48hrs for symptoms to appear. Athlete has a whey/casein protein supplement that they've taken daily for an entire season. Athlete drinks milk with their meals, and eats cheese where applicable (e.g., Chipotle bowls, breakfast omelets, etc..).
How is "athlete" supposed to know that their bloating, rashes, and gas are related to dairy when the IgG symptoms are not instant (like IgE), and they've "been drinking and eating like this forever?"
Being aware of your food triggers is a way to find these "hot spots" of a slow-burning inflammation in your body. Putting out these smoldering flames is an easy way to improve overall health and performance, AND be sure that the athlete would enter a concussion with minimal gut/systemic inflammation. This is important as the gut-brain axis is disrupted within 6-8hrs of a concussion.
*Note: The IgG testing is the least "science-based" recommendation in these 5 tips from a conventional, MD-approved standpoint (the dairy industry doesn't like when you knock it). Snark aside, this is one of the most useful and high-yield changes that many of my athletes have made without us adding supplements or doing anything crazy. We shift a protein power and energy improves, rashes go away, sleep is deeper, etc... All good things.
3. Creatine Monohydrate
Creatine monohydrate is one of the most studied, safe, and efficacious ergogenic ("sports performance") aids available today. It's used by our phosphagen ("burst") energy systems, so traditional it was limited to strength and power athletes.
Newer research is finding that creatine is good for nearly any and all athletes, good for the heart, and good for the brain. Further, after a concussion, brain creatine levels drop. This is because your brain uses creatine as a means for energy during the energy deficit.
By supplementing creatine before an injury, your creatine "reserves" prevent a drastic energy deficit after a concussion. This protects brain function and may minimize symptoms.
So, not only will you get the traditional “sports benefits” of creatine, but you'll also have a small "energy insurance policy" for your brain should a concussion occur.
4. Magnesium
This is another wildly simple, super safe, and high-yield supplement. Magnesium is a mineral used by over 300 enzymatic processes in the body. Helps to produce energy (ATP), proteins, glutathione, etc…
And guess what? MOST people are deficient. Especially, hard-working, sweaty athletes.
Beyond its role as an electrolyte, magnesium may play a role in minimizing excitotoxicity inc concussion. This is because of its role as a “plug” on the glutamate (NMDA) receptor. Fancy neurology there, but that's a receptor that gets overstimulated in concussion and contributes to symptoms and the energy deficit.
Having healthy magnesium levels prior to a concussion can minimize the change for too much excitotoxicity and inflammation in a concussion injury.
5. Omega-3 Fish Oil (EPA/DHA)
Last, but certainly not least, athletes should be taking a fish oil (EPA/DHA) supplement. Why? Because of the beneficial effects on inflammation levels and immune regulation.
This ties beautifully into concussion prevention, as well, because fish oil covers the inflammation box AND the structural box. Your brain is mostly fat, 10-20% of which are omega-3 fats. Further, 97% of that fat (in a healthy person) should be DHA.
What are the benefits of a healthy Omega-3 Index and having adequate EPA/DHA in your system before a concussion?
Protection against reduced plasticity by normalizing protein levels in neuronal circuits associated with learning, cognitive processing, synaptic facilitation, neuronal excitability, and locomotor control.
Reduced markers of injury (e.g., Neurofilament Light, NFL) and apoptosis (“programmed cell death”)
Minimizes white matter damage and preservation of nerve coats (i.e., myelin)
Minimizes glutamate excitotoxicity.
Protect against calcium overload & preserves mitochondria function
In the research, most NCAA athletes do not have adequate omega-3 levels. A test I used in my office, and the test we used to find omega-3 levels in these NCAA athletes, is called the Omega-3 Index. We want 8-11% of your cell membrane to be composed of omega-3s. We find that most elite athletes are around 4-5%.
High-yield summary.
Concussions make up roughly 10-30% of all sports injuries in high school and college.
Even then, roughly 50% of sports-related concussions go unreported.
How do we prevent metabolic damage in these concussions - both reported and unreported?
Dr. Mark Heisig is a licensed naturopathic doctor with continuing mTBI education from The American Academy of Neurology (AAN), Complete Concussion. Management (CCMI) and The Carrick Institute. His office is located in Scottsdale, AZ.




